Key points
If you’ve ever experienced a sleep problem, you’ll know it can be a difficult and isolating experience but it’s not something you need to live with. Despite many people experiencing insomnia for months, even years at a time, it’s actually very treatable.
But, with so many treatment options available, how do you know what’s right for you? There may be countless options out there, but they’re certainly not all equal when it comes to getting the results you want.
In this article we’ll explore the gold standard of insomnia treatments, Cognitive Behavioural Therapy for insomnia (CBTi). We’ll explain:
- what CBTi is and why it’s the best option for treating your insomnia
- how CBTi can help you fall asleep faster and stay asleep longer
- what you can expect during CBTi
- how effective CBTi is for resolving even the most severe insomnia.
Is CBTi the best way to address your sleep problem?
If you’re reading this, you’re probably very familiar with how it feels when you can’t sleep. Lying awake for what may be hours on end, willing sleep to come before you have to face the day ahead, fuelled on barely any sleep and sapped of energy.
And what about when morning does eventually come? Do you find yourself already anxious about the following night, unable to shake the feeling that your sleep will be as bad or even worse than the night before?
When this happens, it can feel like your whole life is being ruled by your lack of sleep.
If this sounds like you, CBTi could be the answer you’ve been looking for.
Cognitive Behavioural Therapy for insomnia (CBTi) is a drug-free treatment for insomnia, helping people take back control of their sleep long-term.
But what actually is CBTi?
First developed in the 1980s, CBTi combines several approaches to help combat difficulties falling and staying asleep.1 2 CBTi takes both a mental and physical approach to addressing your sleep, helping you to overcome:
- inappropriate thought processes
- behaviours that don’t promote healthy sleep.
A lot of people who sleep badly are already doing a whole range of things to promote good sleep. So it can be frustrating if you’ve already tried such techniques as having a wind-down routine or creating the ideal bedroom setup for a great night’s sleep, and still find yourself unable to drift off or wide awake in the small hours.
If you’ve already taken these steps, then why is it that you still can’t sleep?
CBTi not only helps identify external patterns and behaviours that might be stopping you sleeping well, it also helps you to pinpoint any negative thoughts and feelings you may have around sleep.
Once you’re aware of these thoughts and how they’re impacting you, you’ll develop the skills to turn your relationship with sleep around, so that you’re back in control.
CBTi is usually delivered over a course of 6–8 sessions, though meaningful improvement can often be seen after four sessions. During these sessions, you’ll learn to reframe your feelings and thoughts and adjust any of your behaviours that are keeping you from getting a good night’s sleep. We’ll explore these techniques in more detail below.
Get expert support to sort your sleep
Fixing a sleep problem can be tough on your own. And while all CBTi is built on the same foundations, the support you get isn’t. With Sleepstation, you’ll have knowledgeable, empathetic guidance every step of the way from your dedicated sleep team. Offering personalised advice, they’ll help you achieve the goals that really matter to you.
Does CBTi work?
If you’ve had a sleep problem for a while, it might feel like you’ve tried every solution out there. From pills to sleep aids, to the latest sleep hack, each promises to get you to sleep swiftly and soundly.
And if you’re reading this, it’s likely that they haven’t worked, or at least not for any length of time.
So what makes CBTi any different?
Since CBTi was first developed, there’ve been many trials that have shown it to be extremely effective.3 4 5 In fact, the evidence is so positive that it’s now considered the first line treatment for adults with insomnia.6 7 8
The aim of CBTi isn’t to get everyone sleeping the same specific number of hours, as everyone has an individual sleep need. Instead, CBTi aims to help improve your sleep so that you wake rested and feel happier, healthier and more alert during the day.
With CBTi you’ll learn to:
- increase how rested you feel in the morning
- increase daytime alertness
- improve habits that promote sleep
- develop realistic expectations about sleep
- decrease frustrations surrounding sleep
- improve your understanding of sleep, especially how much control you have over your own sleep.
Does CBTi alter sleep architecture?
Sleep architecture is the amount and distribution of the different sleep stages.
Every night, you cycle through several sleep stages, each one carrying out important, different processes to make sure your brain and body perform at their best. The stages are:
- Stage N1
- Stage N2
- Stage N3
- REM sleep.
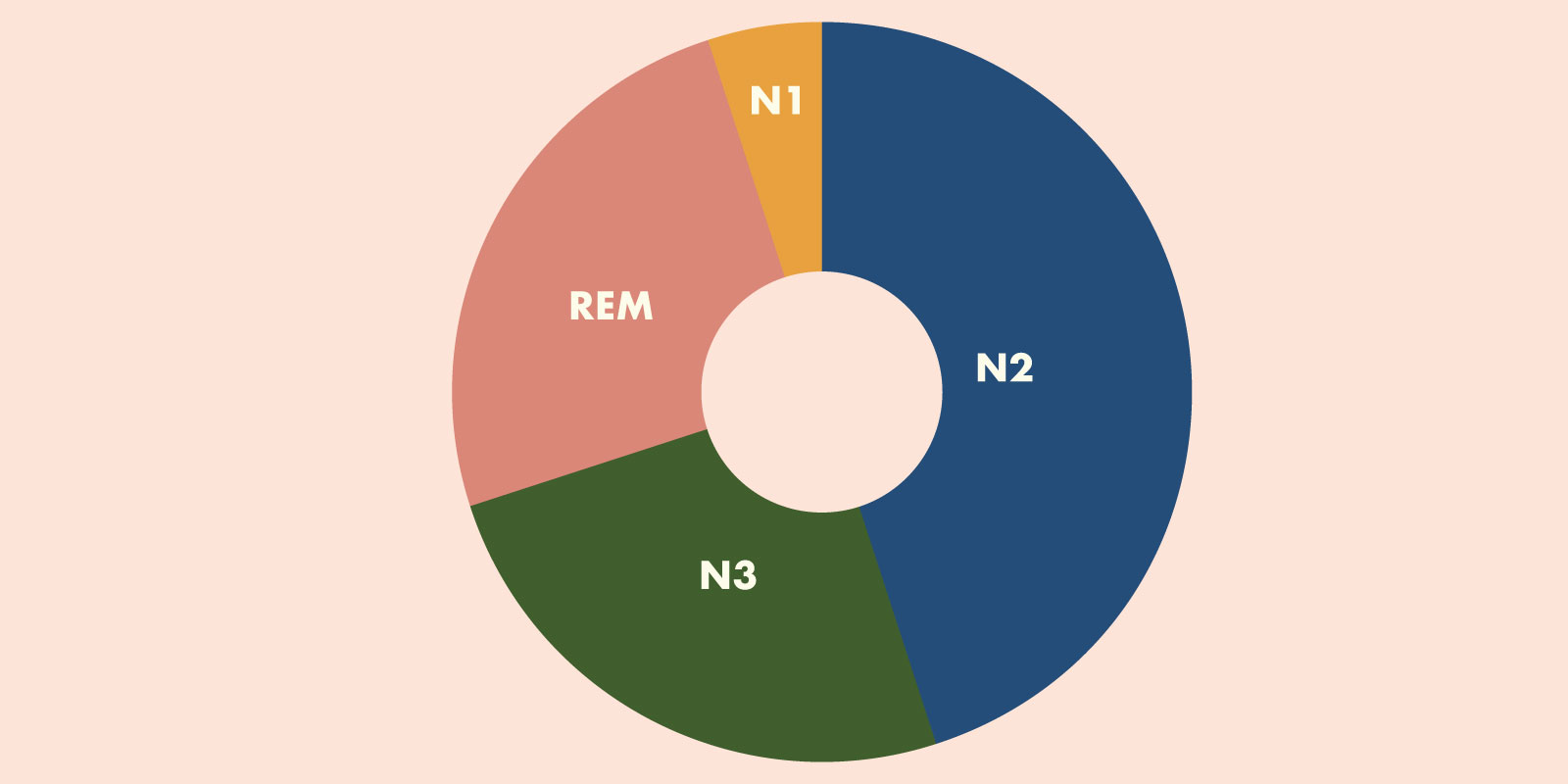
When you’re sleeping badly, this can affect the amount of each sleep stage you get during the night and you can end up feeling the effects of this during the day. Whether you can’t get to sleep or you wake repeatedly during the night, this won’t allow your body to cycle through the necessary stages properly and complete all its vital work.
And if you’re not getting enough good quality sleep, this is going to impact both your physical and mental health.
CBTi doesn’t affect your sleep architecture in itself. But by improving the duration of your sleep and consolidating your sleep periods, your brain can reassert its natural sleep architecture that’s been disturbed by your broken sleep.
So how does CBTi actually achieve this?
Let’s take a look at the different techniques used in CBTi that work together to get your sleep back on track.
The five components of CBTi
CBTi is made up of a range of different techniques, combined to give long-lasting, effective results.9 These techniques include:
- stimulus control therapy
- sleep restriction therapy
- sleep hygiene education
- cognitive therapy
- relaxation training.
But what do these terms actually mean? Let’s find out.
Stimulus control therapy
Many of us use our bedrooms for much more than simply sleeping.
Whether you combine your bedroom with your workspace or binge Netflix on your bed, this can cause your brain to associate your bedroom with far more activities than it should. And this can make it much harder for you to fall asleep.
Stimulus control therapy is all about reassociating the bedroom with sleep.10 11 This is done by following some simple rules:
- only going to bed when you’re sleepy
- limiting activities in bed to sleep (and intimacy)
- getting out of bed at the same time every morning, no matter how much sleep you’ve had
- getting out of bed if you’ve been awake for longer than 30 minutes
- avoiding naps during the day if possible, so that you’re only sleeping at night and in your bed.

Sleep restriction therapy
A lot of people with insomnia have difficulty either falling asleep or staying asleep during the night. If you’ve experienced this, you’ll likely know the frustration of lying awake, staring at the ceiling and unable to get that rest you so desperately crave.
Sleep restriction therapy (SRT) aims to address this problem by limiting the amount of time you spend in bed.12 This can cause mild sleep deprivation and increase the pressure for sleep. This is managed by:
- delaying your bedtime
- establishing a fixed wake up time.
Over a few weeks, your bedtime is gradually modified until you’re getting as much sleep as you can during the shortest time in bed. We measure this using sleep efficiency.
What is sleep efficiency?
Sleep efficiency (SE) is an important measure when it comes to improving your sleep.
It’s measured by dividing your total sleep time by the time you’ve spent in bed. So if you spent eight hours in bed but only four of those hours asleep then your SE would be 50%.
It can actually come as quite a surprise to see just how much time you’re spending in bed awake each night, rather than sleeping.
Over the course of your CBTi, you should see an increase in your SE, with the aim of reaching a final score of 85% or above. This is classed as ‘good’ sleep efficiency and means you’re spending 85% or more of your time in bed asleep.
Does sleep restriction mean less sleep?
You might be wondering if, by spending less time in bed, you’ll be giving yourself less opportunity to sleep so sleep restriction will actually have the opposite effect.
Sleep restriction can feel really counterintuitive at the beginning. Surely less time in bed means less chance to sleep, right?
Actually, no!
Sleep restriction can be tough in the first couple of weeks before the body adapts. It may be the case that you get less sleep during these first weeks and you can experience high levels of daytime sleepiness during this time.
It’s important to remember that this may happen but it’s only a temporary effect. But if you’re worried about this aspect of CBTi, it’s worth having a chat with your GP before you start.
Sleep restriction can significantly improve SE% by helping you to consolidate your broken sleep. So the end result is that you may spend an equal amount or less time in bed than you were, but you’re spending much more of that time asleep.
Sleep hygiene
Sleep hygiene is the idea that you can adjust your habits and adapt your environment for better sleep. What good sleep hygiene looks like, and what’s effective, is very individual and will vary from person to person.
So the goal of sleep hygiene, as part of CBTi, is to identify and encourage these positive sleep-related behaviours and habits to become part of your daily routine.
While sleep hygiene advice and implementing positive sleep practices may be helpful for many people, this approach on its own may not be effective for someone who’s experiencing a sleep problem.13
It’s when you combine the other behavioural therapies used in CBTi with good sleep hygiene that really makes the difference.
What is good sleep hygiene?
Even though there’s no one-size-fits-all approach to sleep hygiene, there are some common suggestions and behaviours that are recommended.
If you want to practise good sleep hygiene, make sure to:
- wake at approximately the same time each day
- get exposure to bright light during the day
- limit napping
- limit or eliminate caffeine, nicotine, alcohol
- go to bed only when sleepy
- take daily exercise
- begin to wind down your day at least one hour before bedtime
- have a comfortable bedroom used only for sleeping and intimacy.9

Cognitive therapy
As mentioned earlier, it’s not just physical behaviours that can keep you up at night. Negative or incorrect beliefs about sleep can also be a big cause of poor sleep. They can cause you unnecessary stress and worry and keep you awake at night.
Cognitive therapy can address a range of beliefs and thoughts, including:
- misconceptions about the cause of insomnia — “Insomnia is a normal part of ageing.”
- unrealistic expectations around sleep need — “I must have eight hours of sleep each night.”
- faulty beliefs about the consequences of insomnia — “Insomnia can make me sick or cause a mental breakdown.”
- myths about what behaviours lead to good sleep — “I can only sleep if I take a sleeping pill.”
Cognitive therapy is designed to educate and reassure you about sleep and teach you to:
- identify incorrect beliefs about sleep
- challenge the truthfulness of these beliefs
- substitute them for realistic thoughts.
These kinds of unhelpful thoughts can actually make your insomnia worse. Research showed that people who claim to have insomnia actually overestimate the time it takes to fall asleep and the amount of disturbances they have during the night. After learning that they were sleeping for longer than they thought, they began to sleep better.14
Relaxation training
Relaxation training helps to reduce arousal and make it easier to get to sleep or to fall back asleep if your sleep has been interrupted. This means engaging in activities that you find relaxing shortly before bed or exercises that can be done when lying awake during the night.15 16
Common relaxation techniques include:
- breathing exercises
- meditation
- progressive muscle relaxation (PMR).
Relaxation training can benefit your sleep on its own but is most effective when combined with the other CBTi techniques mentioned above.
So now we know what CBTi is, how does it compare to other methods of treating insomnia? Are the results more effective than over-the-counter sleep aids or prescribed medication? Let’s find out.
CBTi vs pills
As we said at the beginning of this article, CBTi is now the recommended first line treatment for insomnia. In the past medication was often used in the hope of a quick fix.
But sleeping tablets were only recommended as short-term solutions and carried the risk of unwanted side effects.
If you’re looking for a long-lasting, drug-free solution to your sleep problems, CBTi could be the alternative for you.
CBTi has been shown to be as effective, if not more, than conventional sleeping tablets in reducing the time it takes to fall asleep and increasing your total sleep time. It’s also proven to be equally effective in improving SE%, as mentioned earlier.17 18 19
CBTi also has two major advantages over sleeping tablets.
CBTi has long-lasting effects
As soon as you stop taking sleeping tablets, you lose any benefit you were experiencing to your sleep. Sometimes you can even end up with rebound insomnia, so you’re back where you started before you took the pills. But the positive effects of CBTi can last well after your therapy has finished, for up to a year or even longer in some cases.20 21
CBTi has almost no side effects
Compared with sleeping tablets, CBTi has next to no side effects. In the early stages, you might experience a temporary increase in daytime sleepiness due to the sleep restriction component, but few other side effects have been noted. There’s also no possibility of dependence or addiction forming.
CBTi can help you reduce or stop taking sleep medication
If you’re already taking sleep medicines, CBTi can be beneficial in helping you to reduce the dose or frequency of your medication.
While sleeping pills may help you get to sleep and stay asleep, they only treat the symptoms and can’t get to the root of why you’re sleeping badly. So once you stop taking them, your symptoms can return.
CBTi works differently. It doesn’t just treat the symptoms of a sleep problem, it helps you identify the underlying cause of your poor sleep and equips you with ways to overcome it. In consultation with their healthcare provider many people find that as their sleep improves with CBTi, their use of sleeping pills can be decreased.
In fact, studies have shown that CBTi can actually help people to completely stop using sleep medication.22 23

Who can benefit from CBTi?
CBTi can benefit nearly anyone with insomnia, whatever the cause. Whether your insomnia’s caused by your lifestyle, mental or physical health conditions or another medical issue, CBTi can help improve your sleep.
Can CBTi help other conditions?
A number of medical conditions can impact your sleep. While not treating the primary condition, CBTi has been shown to improve sleep in many physical and mental health conditions.24
By improving your sleep you can aid recovery in a lot of conditions. Better sleep can also help you cope with your illness and even improve treatment outcomes for conditions such as diabetes.25
There’s evidence to show that CBTi has helped improve sleep for people living with many different conditions.
Mental health conditions including:
- anxiety
- social phobia
- depression
- PTSD.24 25 26
Physical health conditions including:
- tinnitus
- pain
- arthritis
- diabetes
- obstructive sleep apnea
- coronary heart disease
- Parkinson’s disease
- multiple sclerosis
- menopause/post-menopause
- cancer. 24 27 28 29 30 31 32 33 34 35
Is CBTi suitable for everyone?
There are a small number of people who wouldn’t be recommended CBTi, including those with epilepsy, mania, parasomnias or people at high risk of falls. This is because certain aspects of CBTi, such as sleep restriction or stimulus control therapy, may make their existing symptoms worse.
Some external factors, such as very irregular shift work may also mean that certain aspects of CBTi are more difficult to follow. If you’re a shift worker and need help with your sleep, this needs to be taken into consideration before you begin CBTi. If you have existing health conditions and are unsure whether CBTi would be a suitable route for you, you should speak to your healthcare provider first.
As we said, though, this is a very small number. The majority of people with a sleep problem are likely to benefit from CBTi. But because of the widespread need for it, there aren’t enough CBTi professionals to meet the demand. So what’s the alternative?
Is digital CBTi as effective as face-to-face therapy?
Digital Cognitive Behavioural Therapy for insomnia (dCBTi) is a form of CBTi where your therapy takes place online, rather than in person.
While CBTi was developed as a face-to-face treatment, dCBTi has been shown to be just as effective as face-to-face therapy.36 37 Avoiding long waiting lists, dCBTi takes place online and means many more people can get the help they need much sooner.
But it pays to be aware that different providers of dCBTi offer different levels of support. Some are fully automated apps, with no input from trained professionals. Sleepstation’s very own digital sleep clinic takes a different approach, including fully human support from dedicated sleep coaches, whose training and expertise makes up an integral part of their dCBTi design.
One study compared various forms of dCBTi with face-to-face CBTi.38 This study showed that dCBTi with a virtual or real ‘therapist’ offers better outcomes than other dCBTi approaches.
This is where Sleepstation can help.

Sleepstation is a world leader in dCBTi
Sleepstation is an online digital sleep clinic that offers dCBTi. Our dCBTi is fully supported by a team of sleep experts, therapists and coaches throughout.38
This means that you’ll have personalised advice and guidance that’s tailored to your specific needs.
With no waiting lists and an entirely online delivery, you can access your sessions at a time and place to suit you. And you can be reassured that there’s someone reading every message, monitoring your progress and cheering you on every step of the way.
We’ve helped thousands of people with sleep problems just like you to take back control of their sleep in just a few short weeks. To get started, just fill in our short sleep quiz to take your first steps on your journey back to better sleep.
Summary
- Cognitive Behavioural Therapy for insomnia (CBTi) is an effective, drug-free solution to sleep problems.
- Using a combination of techniques, it helps you adapt your thought processes and behaviours to fall asleep quicker and stay asleep longer.
- CBTi can improve sleep for people who have a wide range of mental and physical conditions.
- Digital CBTi (dCBTi) is just as effective as face-to-face alternatives.
- Sleepstation combines dCBTi with human support to give you the best chance of taking back control of your sleep for the long-term.
References
- Lacks P. Behavioural treatment for persistent insomnia. Elsevier Science: London, 1987. ↩︎
- Parsons CE, Zachariae R, Landberger C, Young KS. How does cognitive behavioural therapy for insomnia work? A systematic review and meta-analysis of mediators of change. Clin Psychol Rev 2021; 86: 102027. ↩︎
- Muench A, Vargas I, Grandner MA, Ellis JG, Posner D, Bastien CH et al. We know CBT-I works, now what? Fac Rev 2022; 11. ↩︎
- Morin CM, Hauri PJ, Espie CA, Spielman AJ, Buysse DJ, Bootzin RR. Nonpharmacologic treatment of chronic insomnia. Sleep 1999; 22: 1134–1156. ↩︎
- Davidson JR, Dickson C, Han H. Cognitive behavioural treatment for insomnia in primary care: a systematic review of sleep outcomes. Br J Gen Pract 2019; 69: e657–e664. ↩︎
- Insomnia: Management [Internet]. [cited 2023 Sept 20]. Available here. ↩︎
- Riemann D, Baglioni C, Bassetti C, Bjorvatn B, Dolenc Groselj L, Ellis JG et al. European guideline for the diagnosis and treatment of insomnia. J Sleep Res 2017; 26: 675–700. ↩︎
- Edinger JD, Arnedt JT, Bertisch SM, Carney CE, Harrington JJ, Lichstein KL et al. Behavioral and psychological treatments for chronic insomnia disorder in adults: an American Academy of Sleep Medicine clinical practice guideline. J Clin Sleep Med 2021; 17: 255–262. ↩︎
- Morin CM. Cognitive-behavioral approaches to the treatment of insomnia. J Clin Psychiatry 2004; 65 Suppl 16: 33–40. ↩︎
- Bootzin RR. Stimulus control treatment for insomnia. Proceedings of the American Psychological Association 1972; 7: 395–396. ↩︎
- Bootzin RR, Epstein DR. Stimulus Control. In: Treatment of Late-Life Insomnia. Thousand Oaks, CA: SAGE Publications; 2000, p. 167–184. ↩︎
- Spielman AJ, Saskin P, Thorpy MJ. Treatment of chronic insomnia by restriction of time in bed. Sleep 1987; 10: 45-56. ↩︎
- Irish LA, Kline CE, Gunn HE, Buysse DJ, Hall MH. The role of sleep hygiene in promoting public health: A review of empirical evidence. Sleep Med Rev. 2015;22:23–36. ↩︎
- Harvey AG, Sharpley AL, Ree MJ, Stinson K, Clark DM. An open trial of cognitive therapy for chronic insomnia. Behav Res Ther 2007; 45: 2491–2501. ↩︎
- Turner RM, Ascher LM. Controlled comparison of progressive relaxation, stimulus control, and paradoxical intention therapies for insomnia. J Consult Clin Psychol 1979; 47: 500–508. ↩︎
- Means MK, Lichstein KL, Epperson MT, Johnson CT. Relaxation therapy for insomnia: nighttime and day time effects. Behav Res Ther 2000; 38: 665–678. ↩︎
- Okajima I, Komada Y, Inoue Y. A meta-analysis on the treatment effectiveness of cognitive behavioral therapy for primary insomnia: CBT for insomnia: a meta-analysis. Sleep Biol Rhythms 2011; 9: 24–34. ↩︎
- Mitchell MD, Gehrman P, Perlis M, Umscheid CA. Comparative effectiveness of cognitive behavioral therapy for insomnia: a systematic review. BMC Fam Pract 2012; 13. doi:10.1186/1471-2296-13-40. ↩︎
- Kay-Stacey M, Attarian H. Advances in the management of chronic insomnia. BMJ 2016; : i2123. ↩︎
- Ritterband LM, Thorndike FP, Ingersoll KS, Lord HR, Gonder-Frederick L, Frederick C et al. Effect of a web-based cognitive behavior therapy for insomnia intervention with 1-year follow-up: A randomized clinical trial. JAMA Psychiatry 2017; 74: 68–75. ↩︎
- Vedaa Ø, Hagatun S, Kallestad H, Pallesen S, Smith ORF, Thorndike FP et al. Long-term effects of an unguided online cognitive behavioral therapy for chronic insomnia. J Clin Sleep Med 2019; 15: 101–110. ↩︎
- Sweetman A, Putland S, Lack L, McEvoy RD, Adams R, Grunstein R et al. The effect of cognitive behavioural therapy for insomnia on sedative-hypnotic use: A narrative review. Sleep Med Rev 2021; 56: 101404. ↩︎
- Vedaa Ø, Kallestad H, Scott J, Smith OR, Pallesen S, Morken G et al. Digital cognitive-behavioural therapy for insomnia (dCBTI) is associated with improved sleep and less self-report use of sleep medication. . ↩︎
- Smith MT, Huang MI, Manber R. Cognitive behavior therapy for chronic insomnia occurring within the context of medical and psychiatric disorders. Clin Psychol Rev 2005; 25: 559–592. ↩︎
- Hertenstein E, Trinca E, Wunderlin M, Schneider CL, Züst MA, Fehér KD et al. Cognitive behavioral therapy for insomnia in patients with mental disorders and comorbid insomnia: A systematic review and meta-analysis. Sleep Med Rev 2022; 62: 101597. ↩︎
- Tang NKY. Brief CBTI for insomnia comorbid with social phobia: A case study. Behav Cogn Psychother [Internet]. 2010;38:113–22. ↩︎
- Curtis F, Laparidou D, Bridle C, Law GR, Durrant S, Rodriguez A et al. Effects of cognitive behavioural therapy on insomnia in adults with tinnitus: Systematic review and meta-analysis of randomised controlled trials. Sleep Med Rev 2021; 56: 101405. ↩︎
- Selvanathan J, Pham C, Nagappa M, Peng PWH, Englesakis M, Espie CA et al. Cognitive behavioral therapy for insomnia in patients with chronic pain – A systematic review and meta-analysis of randomized controlled trials. Sleep Med Rev 2021; 60: 101460. ↩︎
- Bensen-Boakes DB, Osman A, Lack L, Catcheside P, Antic N, Smith SS et al. The Effect of Cognitive Behavioural Therapy for Insomnia (CBT-I) on Subjective-Objective Sleep Discrepancy in Individuals with Co-Morbid Insomnia and Sleep Apnoea: A Randomised Controlled Trial. Applied Sciences. 2009; 12. ↩︎
- Yang H, Petrini M. Effect of cognitive behavior therapy on sleep disorder in Parkinson’s disease in China: A pilot study. Nurs Health Sci 2012; 14: 458–463. ↩︎
- Rybarczyk B, Mack L, Harris JH, Stepanski E. Testing two types of self-help CBT-I for insomnia in older adults with arthritis or coronary artery disease. Rehabil Psychol 2011; 56: 257–266. ↩︎
- Diem SJ, LaCroix AZ, Reed SD, Larson JC, Newton KM, Ensrud KE et al. Effects of pharmacologic and nonpharmacologic interventions on menopause-related quality of life: a pooled analysis of individual participant data from four MsFLASH trials. Menopause 2020; 27: 1126–1136. ↩︎
- Squires LR, Rash JA, Fawcett J, Garland SN. Systematic review and meta-analysis of cognitive-behavioural therapy for insomnia on subjective and actigraphy-measured sleep and comorbid symptoms in cancer survivors. Sleep Med Rev 2022; 63: 101615. ↩︎
- Majendie CM, Dysch L, Carrigan N. Cognitive behavioral therapy for insomnia (CBTI) for an adult with multiple sclerosis. Clinical Case Studies 2017; 16: 115–131. ↩︎
- Soh HL, Ho RC, Ho CS, Tam WW. Efficacy of digital cognitive behavioural therapy for insomnia: a meta-analysis of randomised controlled trials. Sleep Med 2020; 75: 315–325. ↩︎
- Zachariae R, Lyby MS, Ritterband LM, O’Toole MS. Efficacy of internet-delivered cognitive-behavioral therapy for insomnia – A systematic review and meta-analysis of randomized controlled trials. Sleep Med Rev 2016; 30: 1–10. ↩︎
- Hasan F, Tu Y-K, Yang C-M, James Gordon C, Wu D, Lee H-C et al. Comparative efficacy of digital cognitive behavioral therapy for insomnia: A systematic review and network meta-analysis. Sleep Med Rev 2022; 61: 101567. ↩︎
- Anderson K, Goldsmith P, Gardiner A. A pilot evaluation of an online cognitive behavioral therapy for insomnia disorder – targeted screening and interactive Web design lead to improved sleep in a community population. Nat Sci Sleep 2014; 43. ↩︎