Key points
Figures suggest that around a third of the UK adult population may experience symptoms of insomnia each week.1 What many of us don’t realise is that insomnia responds really well to treatment.
In this article, we’ve outlined how you can access insomnia treatment through the NHS and we’ve covered the following points:
- when you should consider treatment for a sleep problem
- how you can access Sleepstation’s guided self-help programme through the NHS
- different approaches to treating insomnia
- why Cognitive Behavioural Therapy for insomnia (CBTi) is so effective.
Introduction
Sleep problems tend to get worse the longer we leave them so it’s best to tackle a sleep problem as soon as possible.
It’s not always possible to resolve sleep problems by yourself and you may find that you need help from a doctor or support from sleep experts like Sleepstation.
If you’re struggling to get to sleep or stay asleep and it’s affecting your daily life ― particularly if you’ve had the problem for more than four weeks, then it’s time to do something about it.
You may already know that you have insomnia. If not, diagnosis is fairly simple. Most people can be diagnosed with insomnia simply by describing their symptoms. If have or think you have insomnia, Sleepstation could help you determine the cause and overcome your sleep problem.
Accessing Sleepstation through the NHS
It’s best to make sure that we can help you before you register for NHS access. The simplest method to access Sleepstation as an NHS patient is outlined below:
- Click ‘Check NHS availability’ below to begin the process.
- Fill in the box to search for your GP surgery by name, street name, town/city or postcode.
- If NHS access is available for you, register as an NHS patient by completing the online form and we’ll do the rest.
Once your referral form is completed, if your GP thinks that Sleepstation could help you, you’ll be granted access to our NHS service.
Is a GP appointment required?
Not usually. If your GP already knows about your sleep problem and you follow the process outlined above, you shouldn’t need to see your GP to access Sleepstation as an NHS patient.
However, you can also visit your GP in person to discuss your symptoms and insomnia treatment options with them if you’d prefer. Your GP understands your medical history, knows about the other sleep services in your area, and will be able to decide if Sleepstation is the right option for you at this time.
Non-NHS options
Alternatively, if you would like to access Sleepstation immediately – without going via the NHS, you can choose one of our private access options. You’ll be presented with options that are appropriate for you after you complete the questions in the screening questionnaire.
If you purchase one of our private packages, you can request that your results are shared with your GP. Lots of people who buy Sleepstation for themselves like to keep their GP in the loop about the support they’ve had and their improvement.
How effective is Sleepstation?
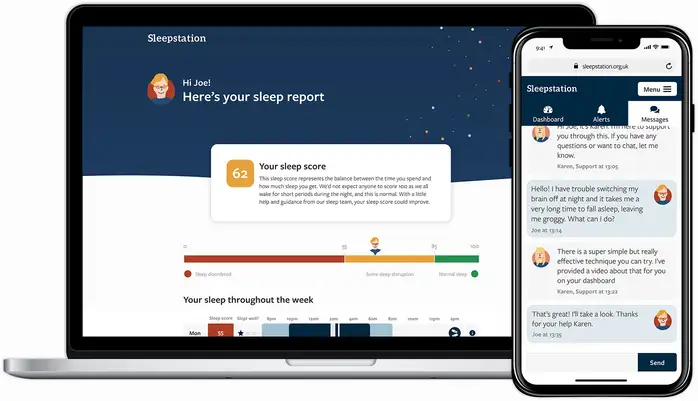
Sleepstation is incredibly effective. Our service has been clinically tested and is proven to help people overcome even very severe insomnia symptoms.2 We continually review the effectiveness of our service and have published our findings in peer reviewed journals.
- Our most recent study showed that, when people follow the advice that we offer through the Sleepstation programme, over 80% gain significant improvement in their sleep as a result.3
- Sleepstation is more effective than sleeping pills with fewer side-effects.
- Sleepstation is more accessible & convenient than insomnia support offered at sleep clinics.
- Most people start to see results within 2–3 weeks using Sleepstation.
- Commitment to the self-help programme is key.
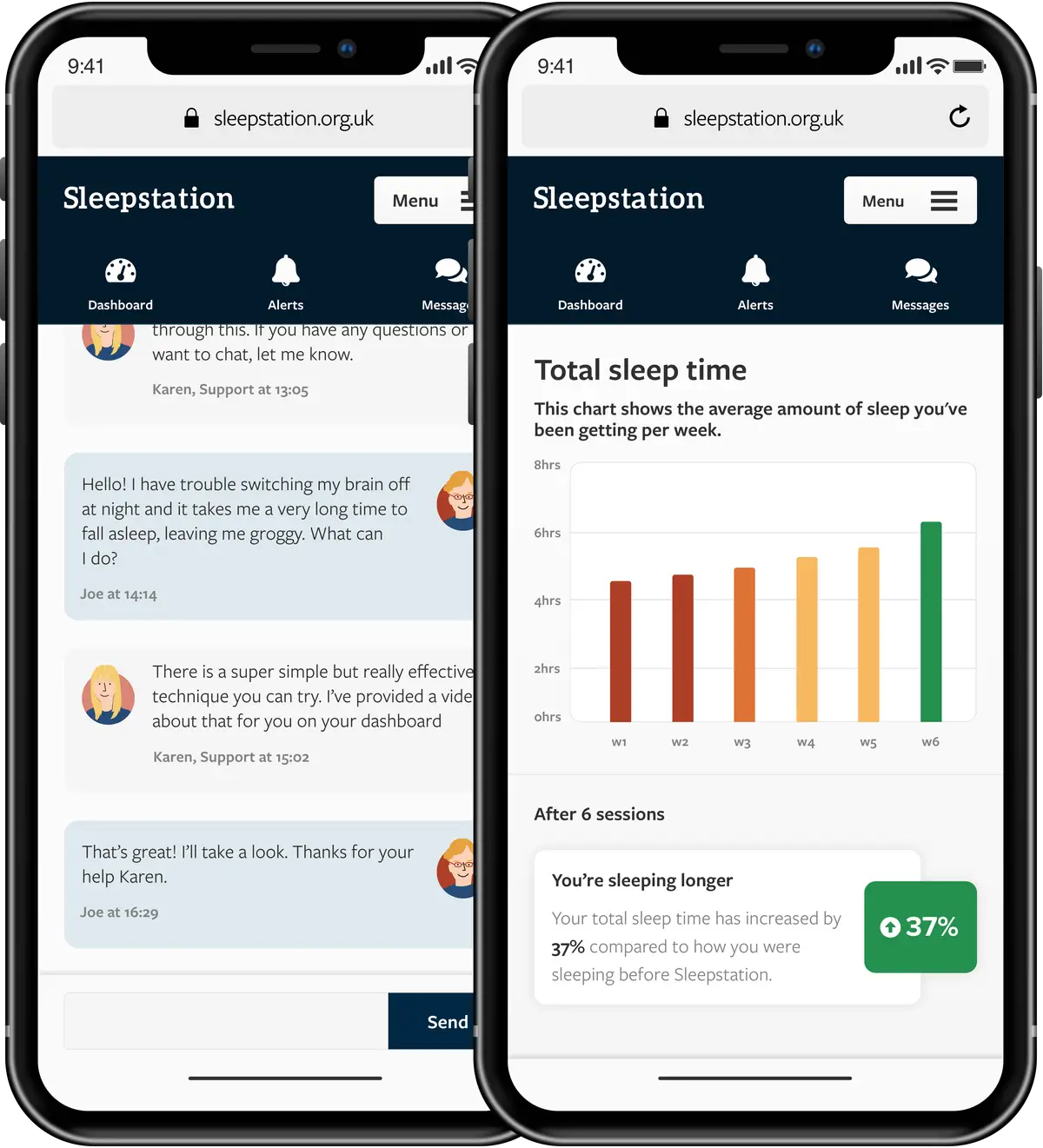
We’ve guided many thousands of people through this programme, and we know that everyone is different. Your sleep problem is unique to you so we’ll tailor your plan to your needs and be available to provide support via our secure messaging system to ensure that you get the best out of your sleep therapy.
Ultimately how effective Sleepstation is depends on you. People who are committed and follow the plan show the greatest improvement. It’s best to start Sleepstation when you feel you’re ready to commit.
What do patients think of Sleepstation?
One former Sleepstation patient is Jan Parsons. Jan had been living with insomnia for many years before trying Sleepstation, in the video below she describes her experience.
Another Sleepstation success story comes from Yvonne, who had experienced over thirty years of disrupted sleep before she found Sleepstation.
Yvonne had been using sleeping tablets for over twenty years, she was exhausted and desperately in need of sleep. Her mental and physical health were being affected and she felt that she’d not had the support she needed to overcome her sleep problem.
Sleepstation not only equipped Yvonne with the tools she needed to take back control of her sleep, we provided her with personalised support every step of the way.
With our help, she reduced her use of sleeping tablets and gained so much confidence in her own ability to get to sleep and stay asleep.
We’re pleased to say that we have a continuous stream of overwhelmingly positive feedback from the thousands of people who have improved their sleep through Sleepstation, from all ages and walks of life.
We maintain regular contract with patients throughout the 6-8 week programme and ask people to share their experiences with us. You can find some more examples of the positive impact Sleepstation can have on our patient stories page.
Insomnia treatments
There are several approaches used to treat insomnia, but the most evidence-based treatment available, the one most widely recommended, is a special type of Cognitive Behavioural Therapy (CBT) designed for people with insomnia.
CBT for insomnia (CBTi)
CBTi is recommended as the best starting point for treating insomnia that has lasted for more than four weeks (chronic insomnia). Unlike sleeping pills, CBTi gets to the root of your sleep problems and offers long-lasting results.
Insomnia often results from stresses and strains in our daily lives coupled with unhealthy lifestyle or sleep habits. CBTi is a sleep therapy that helps you identify and overcome the underlying causes of your sleep problems rather than just reducing the symptoms.
CBTi will help you identify things that could be disrupting your sleep and ways to overcome them. You’ll also look at your sleep habits to ensure your sleep environment and routine are the best they can be to encourage good sleep.
People with insomnia often spend a lot of time lying in bed but not actually sleeping, so another component of CBT can also be sleep restriction.
This is where the time you spend in bed is reduced, to reset your sleep schedule and re-establish the link between bed and sleep. Once you’re sleeping for the majority of the time that you’re actually in bed, sleep time is gradually increased.
So you can see that there’s several components that make up CBTi, but the overall objective is to equip you with the knowledge, tools and skills you need to take back control of your sleep.
CBTi is a highly-effective treatment for insomnia which is proven to have long-lasting results.
There’s a wealth of scientific evidence showing now effective CBTi is. Clinical trials have established that CBTi can improve:
- the quality and quantity of sleep
- how long it takes you to fall asleep
- night-time awakenings
- mental and emotional wellbeing.
CBTi is also recognised as the first line treatment for chronic insomnia by the National Institute of Health and Care Excellence (NICE).4 5
So if it’s recognised as the most effective treatment option, why isn’t it always the first treatment option recommended?
In the UK, a lack of trained sleep therapists and sleep specialists made it very difficult for NHS patients to access CBTi in the past as waiting lists for NHS sleep clinics are incredibly long.
We developed Sleepstation in partnership with an NHS Hospital because we wanted CBTi to be available to as many people as possible on the NHS.
Sleepstation is an online, guided self-help CBTi programme that has been clinically proven to be just as effective as treatment provided in sleep clinics but without the long waiting lists.
The first step in treating insomnia with CBTi is to identify the causes of the insomnia. The Sleepstation programme begins with a week-long self-assessment and sleep diary review.
Sleepstation’s online CBTi programme is available free of charge on the NHS in some areas of the UK. However, you won’t always need to see your GP to get a referral. Further details about the NHS referral options can be found on our NHS options page.
Sleeping pills
Prescription sleeping tablets are usually only considered as a last resort and should be used for only a few days or weeks at a time. This is because they don’t treat the cause of insomnia, they only mask the symptoms.
Sleeping pills come with the risk of developing a dependency and can come with many undesirable side effects6 including:
- daytime drowsiness
- difficulty concentrating
- constipation or diarrhoea
- mood and appetite changes.
They can also become less effective if they’re taken very regularly, so with all these negative points, GPs now rarely prescribe sleeping pills to treat insomnia.

Talking to your GP about your sleep
When you explain your symptoms to your GP, they may start by trying to identify and treat any underlying health condition, such as anxiety, that may be causing your sleep problems.
They may ask you about your sleeping patterns and routines, your daily alcohol and caffeine intake, and your general lifestyle habits, such as diet and exercise. They’ll probably also explain some of the things that you can do to help improve your sleep.7
These include:
- going to bed and getting up at regular times
- taking time to relax before bedtime
- keeping your bedroom cool, dark and quiet
- avoiding caffeine, nicotine, alcohol, heavy meals and exercise in the 2-3 hours before bedtime
- not watching TV or using phones, tablets or computers shortly before going to bed
- avoiding napping during the day
- making a list of your worries, and any ideas about how to solve them, before going to bed to help you put them to the back of your mind until morning

They will also check your medical history for any illness or medication that may be causing or contributing to your sleep problem and should discuss all your treatment options with you. Your views and preferences should always be taken into account when making decisions about your treatment.
Referrals to sleep clinics
An assessment in an NHS sleep clinic is sometimes needed to fully understand and treat sleep problems but there are few specialist centres and waiting lists can be very long.
If your GP decides that a sleep clinic referral is necessary, you will need to attend a specialist sleep clinic or hospital department that provides treatment for people with sleep disorders.
NHS sleep clinics are staffed by highly trained teams of sleep specialists and sleep therapists, in purpose-build clinics with facilities for monitoring sleep.
If you’re referred to a sleep clinic you may be asked to spend the night in a sleep lab so that your sleep can be monitored. While you sleep, the pattern and depth of your sleep will be measured and your breathing and heart rates will be closely monitored.
This is what’s known as a sleep study, or polysomnography. For most people, this can be carried out at home using much simpler monitoring, following demonstration of the equipment during a brief visit to the hospital.
The information gathered during the study can be used to accurately diagnose your sleep problem and can also be used to assess how certain treatments are working, if you’ve already been diagnosed with a sleep problem.
How do I find sleep clinics near me?
You can search online for your nearest sleep clinic, but you’ll need a referral from your GP to access a sleep clinic on the NHS. It’s worth discussing your sleep problem with your GP first as they will know your medical history and how it may be affecting your sleep.
Given that waiting lists for NHS sleep clinics can be long, it might be tempting to look for private sleep clinics near you, however these can be expensive options.
Did you know?
Latest data from the National Institute for Health and Care Excellence (NICE) indicates that around a third of all adults in Western countries experience sleep problems at least once a week and up to 10% of these people would fit the criteria for having insomnia.
Sleep therapists and specialists
The language around treatment for sleep disorders can get confusing, but if you’ve come across the term sleep therapist it’s mostly used to describe someone who provides therapy to help you sleep.
Sleep therapy is another term often used to describe cognitive behavioural approaches to treating insomnia and a sleep therapist is somebody who can provide this type of treatment.
A sleep specialist is generally used to describe a doctor who can diagnose and treat sleep disorders.
Alternative therapies
Some people have reported that alternative therapies such as acupuncture, acupressure, reflexology and hypnosis have been useful in helping them relax and improve sleep.
At the moment, there’s not much scientific proof that they help8 but if you personally find that they help you to relax and unwind then there’s no harm in including them in your routine.
Do you want your GP to refer you to Sleepstation?
Many people have heard about Sleepstation from friends or relatives who have completed the programme and they want to find out how to be referred for NHS access. If that’s why you’re here, you can click the button below to start the process.
Summary
- Insomnia is a very common but highly treatable sleep disorder.
- Different treatment options are available but the gold-standard is CBTi.
- Sleepstation’s guided self-help CBTi programme is clinically proven and highly effective for insomnia symptoms.
- You can see if you can access our service through the NHS in just a couple of clicks.
Start fixing your sleep problem today
References
- CBTi Prevalence | Background information | Insomnia | CKS | NICE [Internet]. Cks.nice.org.uk. 2022 [cited 4 February 2022]. Available here. ↩︎
- Anderson KN, Goldsmith P, Gardiner A. A pilot evaluation of an online cognitive behavioral therapy for insomnia disorder-targeted screening and interactive Web design lead to improved sleep in a community population. Nature and science of sleep 2014; 6. ↩︎
- Gardiner A, Stanley N. 0527 the uptake of a free digital CBTi programme in a large commercial organisation. Sleep 2020; 43: A201–A202. ↩︎
- Scenario: Managing short-term insomnia (< 3 months) | Management | Insomnia | CKS | NICE [Internet]. Cks.nice.org.uk. 2022 Available here. ↩︎
- Scenario: Managing long-term insomnia (> 3 months) | Management | Insomnia | CKS | NICE [Internet]. Cks.nice.org.uk. 2022 [cited 4 February 2022]. Available here. ↩︎
- Evidence context | Hypnotics | Advice | NICE [Internet]. Nice.org.uk. 2022 [cited 4 February 2022]. Available here. ↩︎
- Stepanski EJ, Wyatt JK. Use of sleep hygiene in the treatment of insomnia. Sleep Med Rev 2003; 7: 215–225. ↩︎
- Gooneratne NS. Complementary and alternative medicine for sleep disturbances in older adults. Clin Geriatr Med 2008; 24: 121–38, viii. ↩︎