Key points
In this article, we’re going to explore the antidepressant, amitriptyline, and look at why it’s been used as an insomnia treatment. We’ll cover the following points:
- what type of drug amitriptyline is and what it’s used for
- the side effects of amitriptyline
- how it works to make you sleep
- whether you should you take amitriptyline for insomnia
- whether it’s a good treatment option for insomnia.
Introduction
The drug amitriptyline (also known as amitriptyline HCl or by the brand names Elavil, Endep, Entrip and Trepiline) is one of a class of drugs that are not primarily sleeping tablets but can be used ‘off-label’ to treat insomnia.
This is because amitriptyline can have a sedative effect on those who take it. Traditional sleeping tablets come with the risk of developing tolerance or addiction so GPs often look to drugs like amitriptyline as safer alternatives.
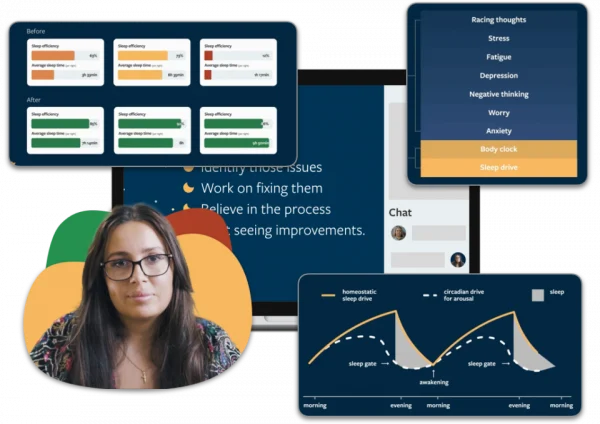
Sleep better without amitriptyline
People who have sleeping problems often turn to amitriptyline, hoping for a quick fix. Most people don’t realise that there are more effective ways to treat your sleeping issues without side effects. With Sleepstation you can significantly improve your sleep without relying on medication. Sleepstation will help you:
- fall asleep quickly
- get all the sleep you need
- spend less time awake in bed
- wake feeling refreshed.
Sleep better without amitriptyline
Get support from sleep experts, plus self-help tools.
Working with an expert who really grasps your situation is key to unlocking real sleep, effortless sleep. You deserve to sleep well and to work with people who have the right knowledge and expertise to help you get there.
Begin your journey to a lifetime of better sleep with:
- a full week of unlimited access to our highly-trained sleep coaches.
- direct contact and professional advice, with no waiting lists.
- expert insights to control and repair your sleep.
- lifetime access to an ever-growing library of sleep tools and resources.
Amitriptyline has multiple clinical uses
Amitriptyline has been around since the 1960s and was originally developed to treat depression. While its popularity in treating depression has declined over the years, it’s become increasingly prescribed for the treatment of insomnia.
In the UK, it’s licensed as an antidepressant and is prescribed to treat:
- major depressive disorder (MDD)
- nerve pain (neuralgia) and back pain
- migraines and tension headaches.
You can find additional information on this drug from the NICE website.

Amitriptyline dosage for sleep, pain relief and mood regulation
Amitriptyline is available in either tablet or liquid form. Both are available in three different strengths: 10mg, 25mg or 50mg. Your doctor will usually start treatment at the lowest possible dose (10mg) and increase it as necessary.
Amitriptyline is used at higher doses for the treatment of depression and low mood (50mg-200mg per day) and at lower doses to treat pain and prevent migraines (10-75mg per day).
The dosage of amitripyline for insomnia treatment is at the lowest end of the scale, typically within the range of 10-25mg per day.
Amitriptyline side effects
When this drug is taken as a sleep aid, the dosage is fairly low, so side effects are generally minimal. There are, however, many potential side effects associated with this medication. The most common amitriptyline side effects include:
- dizziness
- dry mouth
- constipation
- headache
- weight gain.
Serious amitriptyline side effects are generally rare and can include:
- a rapid or irregular heartbeat
- shortness of breath
- chest pain.
If you experience these symptoms, you should contact your healthcare provider immediately.
Subscribe for sleep tips
"*" indicates required fields
Amitriptyline for pain
Low doses of amitriptyline are commonly used for long periods in many people with chronic illness, particularly those with pain syndromes.1 This takes advantage of the fact that the drug has an effect on two chemical messengers, noradrenaline and serotonin, that are found in nerves and between nerve endings.
When you feel pain, these messengers relay signals to the brain that tells it that you’re in pain. When given to treat pain, amitriptyline blocks these two chemical messengers from relaying pain signals to the brain, so pain is reduced.
If you take amitriptyline at night to relieve pain, you may sleep better but that doesn’t mean that the drug is improving your sleep. It may be helping you get to sleep by reducing the pain that was keeping you awake but the drug itself is not, necessarily, having a direct effect on your sleep.

While we know that amitriptyline can be effective in the treatment of pain2 3, its beneficial effects on sleep are much less clear. In fact, the drug may even have a negative effect on sleep, when taken for pain management.4
One treatment that is proven to be effective in treating insomnia for people with chronic pain is cognitive behavioural therapy for insomnia (CBTi).
This treatment has been shown to improve self-reported insomnia symptoms in people with chronic pain, with the improvement in sleep being maintained after the therapy itself has finished.5 In this study, CBTi also reduced pain symptoms in about a third of the trial participants.
CBTi is the gold-standard approach for treating insomnia and it’s what we use here at Sleepstation. So, if you’re experiencing insomnia associated with chronic pain, we may be able to help. Find out, by taking our sleep quiz, how we can help you to improve your sleep.
Amitriptyline: the difference between sleep and sedation
Given that this drug is often prescribed by GPs for the treatment of insomnia, it may come as a surprise to learn that very few studies have actually looked at how amitriptyline affects sleep.
The theory behind its use is that as amitriptyline can make you feel sleepy, it can help you to fall asleep and stay asleep. However, sedation and sleep induction are not the same things.
While sedation may play a role in helping you get to sleep, giving a feeling of restfulness or relaxation, drugs that cause sedation do not put you to sleep or keep you asleep.
Your sleep is controlled by two factors: your body clock and your sleep need. The need for sleep increases steadily over the course of the day. At the same time, your body clock is responsible for telling your brain when it’s time for you to sleep.
In normal, unmedicated sleep, by bedtime your sleep need is high and you’re ready to go to sleep. Your body clock sends chemical signals that tell your body to go to sleep, stay asleep and then, the next morning, wake again.
When sleep is achieved through sedation, this process is very different. Drugs like amitriptyline increase the concentrations of certain chemical signals in the brain and the result is that you feel sleepy quite rapidly after taking it and then hopefully stay asleep during the night.
How long does it take for amitriptyline to work?
This is a very popular question and it really depends on what the drug is being used for. When amitriptyline is taken for sleep, it may make you sleepy within a couple of hours of taking it for the first time or it may take one to two weeks for the effects of the drug to build up enough to have an effect on your sleep.
It will depend on the starting dose of amitriptyline and on how your body individually metabolises the drug and this will vary from person to person.
It’s advised to take amitriptyline a couple of hours before you want to go to sleep. This way, the sedative effects shouldn’t persist when you wake up.
When taken for anxiety, depression or pain-relief, the effects may take several weeks to become noticeable.
Taking amitriptyline for sleep can affect your waking hours
The drawback of this drug-induced sleep is that amitriptyline doesn’t just make you feel sleepy at night. This is because of how long amitriptyline stays in your system. It remains active in the body for 12-24 hours so it can make you feel tired and groggy during the day too.
This effect of the drug has been extensively studied and it’s known that even at low doses amitriptyline causes daytime sedation and has a significant negative effect on daytime cognitive and psychomotor performance.5 6 7 8
This means that it can cause you to feel groggy or make you more clumsy which can affect your ability to carry out normal activities of daily living and can also impact your ability to drive.

The side-effect of daytime sleepiness often leads the person to believe that they’re having problems sleeping. In fact, their daytime sleepiness is directly resulting from the drug they’re taking to help them sleep.
So it’s easy to see that this would be a big drawback to using amitriptyline as a sleep aid. This drug-induced sedation could actually result in a person being given more medications to help them with their assumed sleep problem when, in fact, they don’t actually have one.
Amitriptyline affects sleep quality
In normal sleep, our bodies cycle through different sleep stages. We go through four sleep stages from light sleep to deep sleep and this repeats several times during each night.
When sleep is induced by amitriptyline, sleep stages are disrupted. As mentioned previously, amitriptyline is a tricyclic antidepressant and this category of drugs is known to suppress the deepest stage of our sleep: rapid eye movement (REM) sleep.
REM sleep is important as it’s the stage in which the brain processes emotional information that we’ve experienced during the day. This stage is also thought to be when many types of memories are consolidated and laid down by our brains.
So for people taking amitriptyline this stage can be shortened. Emotional processing may be affected which can leave some users with feelings of anxiety and depression. This is why, when prescribed for insomnia, it’s very important to start with the lowest possible dosage.
Amitriptyline also reduces the amount of deep, slow-wave sleep (SWS), also referred to as ‘deep sleep’. During SWS our bodies are in housekeeping mode: our muscles repair themselves and new tissue is grown.
This type of sleep is considered key to restoring our bodies physically but it’s also important for the consolidation of memories. Not getting enough SWS sleep can leave you feeling fatigued in the short-term and can lead to serious illness in the long-term.

So can amitriptyline help you sleep?
Surprisingly, there’s little, if any, evidence that amitriptyline can improve getting to sleep, staying asleep or any other aspects of sleep architecture relevant to disturbed sleep.9 10 11 12
Because of its effect on SWS, some researchers have expressed concern about the use of amitriptyline to improve sleep, particularly for people experiencing chronic pain. For instance, Drewes et al.,4 stated:
During amitriptyline and opioid treatment, a negative sleep profile may be induced, which can limit the use of these drugs in patients with pain.
This is because both amitriptyline and opioid medications can cause a reduction in SWS and it’s been shown that a reduction in this deep, restorative sleep causes an increase in the perception of pain.13
There are no published studies on the effectiveness of low-dose amitriptyline in insomnia either.1 Yet this drug remains highly prescribed by GPs as a safer alternative to traditional sleeping tablets.
Taking a prescribed sleep aid such as amitriptyline will not help to get to the root cause of a sleep disorder like insomnia. It will only mask the problem and can even make it worse.
This is where Sleepstation differs from medication treatment options for insomnia. Sleepstation is totally medication-free and requires only your ability to commit to following the programme. So with no wonder drugs involved, how do we succeed?
We use the gold-standard approach that’s proven to resolve all forms of insomnia ― cognitive behavioural therapy for insomnia (CBTi). Using CBTi, we’ll help you get to the root of your sleep problem and give you the guidance needed to improve your sleep for good.
You learn key sleep techniques and we provide you with the most up-to-date sleep science, equipping you with the tools to build a solid foundation for good sleep. We then help you to rebuild your sleep, step by step, brick by brick, to get you back to enjoying good-quality, restful sleep.
Our latest data shows that 84% of people using our service report recovery from their sleep problems after completing the course. So if you’re struggling with your sleep and want a clinically-validated, medication-free approach to overcoming your sleep problem, Sleepstation’s digital sleep clinic offers a range of services to fit the severity of your sleep problem and the level of support you need. Get started today.
Summary
- Amitriptyline is widely prescribed as a sleep aid for people with insomnia.
- There is a distinct lack of evidence that amitriptyline has any beneficial effect on sleep in insomnia.
- It can cause daytime sleepiness and grogginess, which can interfere with daily life.
- It can reduce the overall quality of sleep in those who take it.
- It does not treat the root cause of the problem and so is not a good long-term treatment for insomnia.
Let us help you get your sleep back on track
- Improve your sleep in four weeks
- Stay asleep longer
- Get better quality sleep
- Boost your mood
- Sleep medication-free
- Scientifically proven

References
- Wilson S, Anderson K, Baldwin D, Dijk D-J, Espie A, Espie C, et al. British Association for Psychopharmacology consensus statement on evidence-based treatment of insomnia, parasomnias and circadian rhythm disorders: An update. J Psychopharmacol. 2019;33(8):923–47. ↩︎
- Mercadante S, Arcuri E, Tirelli W, Villari P, Casuccio A.Amitriptyline in neuropathic cancer pain in patients on morphine therapy: a randomized placebo-controlled, double-blind crossover study. Tumori. 2002 May-Jun;88(3):239-42. ↩︎
- Watson CP, Chipman M, Reed K, Evans RJ, Birkett N. Amitriptyline versus maprotiline in postherpetic neuralgia: a randomized, double-blind, crossover trial. Pain. 1992 Jan;48(1):29-36. ↩︎
- Drewes AM, Arendt-Nielsen L. Pain and sleep in medical diseases: interactions and treatment possibilities (A review). Sleep Research Online. 2001;4(2):67-76. ↩︎
- McCrae CS, Williams J, Roditi D, Anderson R, Mundt JM, Miller MB, et al. Cognitive behavioral treatments for insomnia and pain in adults with comorbid chronic insomnia and fibromyalgia: clinical outcomes from the SPIN randomized controlled trial. Sleep [Internet]. 2019;42(3) ↩︎
- Srisurapanont M, Jarusuraisin N. Amitriptyline vs. lorazepam in the treatment of opiate-withdrawal insomnia: a randomized double-blind study. Acta Psychiatr Scand. 1998 Mar;97(3):233-5. ↩︎
- Holmberg G. Sedative effects of maprotiline and amitriptyline. Acta Psychiatr Scand. 1988 May;77(5):584-6. ↩︎
- Bye C, Clubley M, Peck AW. Drowsiness, impaired performance and tricyclic antidepressants drugs. Br J Clin Pharmacol. 1978 Aug;6(2):155-62.
↩︎ - Hindmarch, I., Harrison, C. and Shillingford, C.A., 1988. An investigation of the effects of lofepramine, nomifensine, amitriptyline and placebo on aspects of memory and psychomotor performance related to car driving. International clinical psychopharmacology, 3(2), pp.157-165 ↩︎
- Raigrodski AJ, Christensen LV, Mohamed SE, Gardiner DM. The effect of four-week administration of amitriptyline on sleep bruxism. A double-blind crossover clinical study. Cranio. 2001 Jan;19(1):21-5. ↩︎
- Mertz H, Fass R, Kodner A, Yan-Go F, Fullerton S, Mayer EA. Effect of amitriptyline on symptoms, sleep, and visceral perception in patients with functional dyspepsia. Am J Gastroenterol. 1998 Feb;93(2):160-5. ↩︎
- Zitman FG, Linssen AC, Edelbroek PM, Stijnen T. Low dose amitriptyline in chronic pain: the gain is modest. Pain. 1990 Jul;42(1):35-42. ↩︎
- Onen SH, Alloui A, Gross A, Eschallier A, Dubray C. The effects of total sleep deprivation, selective sleep interruption and sleep recovery on pain tolerance thresholds in healthy subjects. Journal of sleep research. 2001 Mar 4;10(1):35-42. ↩︎