Key points
Our daily worries can often creep into our thoughts at night-time and this can seriously disturb our sleep. In this article we’re going to explore ways to calm your weary mind, how to stop overthinking and banish unwanted thoughts from your sleeptime. We’ll cover:
- why shutting out your thoughts and feelings is not a good strategy
- techniques that can help to quieten a racing mind
- how to stop intrusive thoughts at night
- how Cognitive Behavioural Therapy for insomnia (CBTi) equips you to deal with sleep-intruding scenarios.
Introduction
Modern life isn’t easy, with concerns about money, housing, work, relationships and living a “successful” life being frequently reported as sources of worry for many people.
Sometimes our worries can have a real impact. We can’t sleep, overthinking about every little thing.
Frequently, people living with stress, anxiety, depression and insomnia will say that racing, intrusive (unwanted) thoughts make it harder for them to get to sleep than any sort of physical discomfort or pain.1
Insomnia and overthinking often go hand-in-hand. So people with insomnia will commonly try to shut out thoughts that are stopping them from sleeping. This might sound sensible at first, but it can cause more problems than it solves.2 3
By implementing better ways to deal with intrusive thoughts, the time between getting into bed and falling asleep needn’t be so difficult. You may also find it easier to fall back to sleep if your sleep isn’t interrupted by racing, intrusive thoughts.
There are a number of thought blocking strategies that have been studied for dealing with these intrusive thoughts in the context of insomnia. Many will be covered in a course of CBT for insomnia (CBTi).4 5 6
The core of these strategies is that they enable a person to substitute thoughts that might keep them awake (arousing thoughts) with non-arousing thoughts. This should:
- reduce the time it takes to fall asleep (the sleep onset time)
- help you to stop overthinking
- increase sleep quality.
We’ll go over a few of these strategies here, in the hope that they’re useful to you or someone you know.
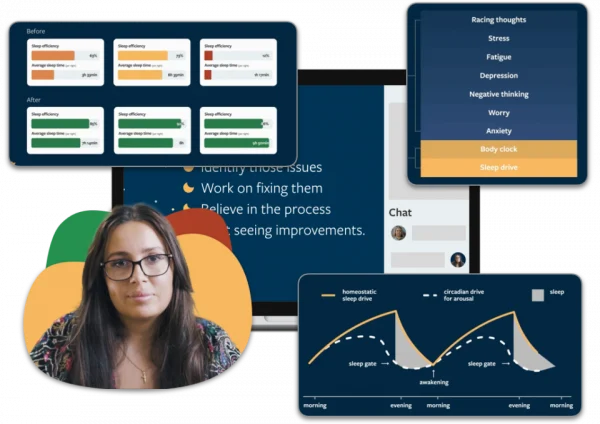
Can’t sleep? Our CBTi programme can help you calm your racing thoughts.
We’ll work with you to get to the root of what’s keeping you awake.
Sleepstation is:
- supported by sleep coaches
- individually tailored to you
- delivered entirely online
- more effective than medication
- clinically proven and accredited by the NHS
Going beyond counting sheep: what to do with unwanted thoughts?
Repeat a word or do a mental puzzle
One of the early, but effective solutions to overthinking and intrusive thoughts in bed is called “articulatory suppression,” in which you would mouth a word at a rate that makes thinking about any other thought difficult ― usually 3 to 4 times a second.
The underlying psychology is complex, but the theory is that mouthing a word requires a lot more mental power than just thinking it and the use of that mental power causes a blocking of the original intrusive thought. Choices of word for this method include:
- the word “the”2
- a nonsense syllable (such as pah, oop, vee.. the choices are endless!)
- a proper name (e.g. Paris, April, Jaffa Cake).
The only requirement is that it has no emotional significance to you (i.e. is non-arousing). You can also extend the technique by:
- accompanying the word you use with a visualisation of a shape, like a triangle or square. This is particularly useful if your intrusive thoughts have a visual component.7
- adding a puzzle element, such as counting back from 1000 in certain “jumps” e.g. 1000, 993, 986, using “jumps” of 7 in addition to using a word, image or syllable.
Since everyone is different, it might take a few goes to find a process which works for you.

Distract yourself
“Imagery distraction” is a helpful technique when you can’t sleep, where you imagine yourself in an engaging and interesting scenario like:
- a relaxing holiday
- cooking a meal or
- a nice, sunny afternoon in the garden.
Although there’s less evidence to suggest imagining a scenario reduces how long it takes to get to sleep compared to articulatory suppression, using mental imagery has been reported to increase the quality of sleep once a person is asleep.8 9
Once you’ve chosen your scenario, the aim is to immerse yourself in it as deeply as possible by imagining all the sights, sounds, smells and ultimately relaxation that comes with it, so that it becomes impossible to think of anything else.
It’s important to avoid scenarios that are too arousing, like a sporting event or sexual encounter, because these scenarios are unlikely to be relaxing and so will make you feel more awake rather than helping you get to, and stay asleep.
Be grateful
Since negative thoughts are often cognitively arousing, fixating on them can make insomnia worse. It’s interesting to note that:
- in one study, subjects who were asked to focus on their regrets at bedtime took longer to get to sleep than those that did not.10
- in another study, participants with insomnia experienced sleep benefits when they focussed on positive thoughts and things they were grateful for at bedtime.9 11
Going over the good things in life may be more difficult for some people than others, such as those with depression12 or anxiety. Specialised treatment should be sought for these conditions.
Accept your thoughts
As strange as it sounds, not doing anything about your intrusive thoughts can be a surprisingly effective strategy to deal with them.
Here, the key is simply to accept that you aren’t able to sleep because of overthinking or intrusive thoughts. By not worrying about the implications, or trying to fight your own thoughts, their impact is dulled which means they’re less liable to be arousing and to keep you awake.2
CBTi can help you take control of your thoughts
These strategies, while effective on their own, are even more effective as part of a structured CBTi programme.5 If you’ve tried multiple techniques and nothing has worked you may need support from an expert sleep team.
At Sleepstation, we developed a digital CBTi programme which has been clinically-validated and is highly effective at resolving insomnia. We’ve helped thousands of people to take back control of their sleep and our results speak for themselves.
So if you can’t sleep at night due to overthinking, our sleep improvement programme can help you optimise your sleep for better health. Get started today.
Summary
- If overthinking or intrusive thoughts are stopping you from sleeping, there’s a range of techniques you can try to clear your mind.
- You could try repeating a word (articulatory suppression), doing a mental puzzle or distracting yourself (articulatory suppression).
- If you’ve tried all of the above options and nothing is working, Sleepstation’s CBTi programme may be able to help you.
References
- Harvey AG. I Can’t Sleep, My Mind Is Racing! An Investigation of Strategies of Thought Control in Insomnia. Behav Cogn Psychother. 2001 Jan;29(1):3–11. ↩︎
- Espie CA. Overcoming Insomnia: A Self-Help Guide Using Cognitive Behavioural Therapy. London, UK: Robinson; 2006. ↩︎
- Schmidt RE, Harvey AG, Van der Linden M. Cognitive and Affective Control in Insomnia. Front Psychol 2011;2:349. ↩︎
- Gellis LA, Park A. Nighttime Thought Control Strategies and Insomnia Severity. Cogn Ther Res 2013 Apr;37(2):383–9.
↩︎ - Harvey L, Inglis SJ, Espie CA. Insomniacs’ reported use of CBT components and relationship to long-term clinical outcome. Behav Res Ther 2002;40:75–83. ↩︎
- Trockel M, Manber R, Chang V, Thurston A, Taylor CB. An e-mail delivered CBT for sleep-health program for college students: effects on sleep quality and depression symptoms. J Clin Sleep Med 2011 Jun 15;7(3):276–81. ↩︎
- Levey AB, Aldaz JA, Watts FN, Coyle K. Articulatory suppression and the treatment of insomnia. Behav Res Ther 1991;29:85–9. ↩︎
- Harvey AG, Payne S. The management of unwanted pre-sleep thoughts in insomnia: distraction with imagery versus general distraction. Behav Res Ther 2002;40:267–77. ↩︎
- Digdon N, Koble A. Effects of constructive worry, imagery distraction, and gratitude interventions on sleep quality: A pilot trial: Effects of interventions on sleep quality. Appl Psychol Health Well Being 2011;3:193–206. ↩︎
- Schmidt RE, Van der Linden M. Feeling Too Regretful to Fall Asleep: Experimental Activation of Regret Delays Sleep Onset. Cogn Ther Res 2013 Aug;37(4):872–80. ↩︎
- Wood AM, Joseph S, Lloyd J, Atkins S. Gratitude influences sleep through the mechanism of pre-sleep cognitions. J Psychosom Res 2009 Jan;66(1):43–8. ↩︎
- Malmberg M, Larsen JK. Depressive Symptoms: The Interaction between Rumination and Self-Reported Insomnia. Depress Res Treat 2015;2015:1–4. ↩︎