Key points
Sleep restriction therapy is a technique commonly used in the treatment of insomnia. It involves a high level of commitment from the person undertaking it but sleep restriction is highly effective and can be very successful in helping to realign and reestablish good sleep.
In this article we’re going to cover:
- the theory behind sleep restriction therapy
- how long does sleep restriction therapy take to work?
- our tips to help you stay the course
- the benefits of sleep restriction therapy.
Good sleep is vital for overall health and wellbeing
Recent research shows that insomnia affects as many as 40% of adults and can be chronic in up to 22% of the population.1 This means that a lot of people experience fragmented, poor quality sleep.
Because of how important sleep is to overall health, it’s not surprising that poor sleep can lead to things like:
- decreased performance across a number of tasks, like driving or working
- general psychological distress
- the worsening of depressive or anxious feelings.
With symptoms like these, lots of people try to get better sleep via increased alcohol consumption, prescription drugs or over-the-counter remedies.2
Although these strategies might work in the short term, they aren’t permanent solutions and come with their own problems such as side effects and addiction risk.
What would be better is a long-term, drug-free approach, tailored to each individual.
One of the most effective medication-free techniques to improve sleep over time is called sleep restriction therapy and is usually offered as part of a Cognitive Behavioural Therapy for insomnia (CBTi) programme. Let’s have a look at what it’s all about.
How does sleep restriction therapy work?
When you have insomnia, you can find yourself spending a lot of time lying in bed awake. This unwanted awake time gives you a lot of time to think and often, these thoughts can become quite negative.
Sleep restriction therapy is based on the idea that when someone with insomnia spends a lot of time awake in bed, they can form a negative set of beliefs about going to sleep (e.g. thinking “I’ll never be able to get to sleep!” or “Why is my sleep so broken?”) and that having those beliefs makes falling and staying asleep harder.
This is because when you go to bed dreading the time you’ll spend lying awake, once there you can find yourself:
- unable to sleep due to the resulting worry
- reinforcing your negative beliefs about sleep.
This “worry pattern” makes it harder to get to sleep, making you more worried, which in turn makes it harder to get to sleep, and so on. Addressing these beliefs can help your recovery from insomnia.
By intentionally limiting how long you spend in bed and inducing mild sleep deprivation, two things happen:
- you fall asleep more readily once in bed because sleep deprivation leads to deeper sleep with a faster sleep onset3
- getting higher quality sleep helps you to challenge the negative beliefs you had about sleep.
So because you’re sleeping better, the negative beliefs you had about sleep are no longer true. Think back to one of the examples of negative thinking we gave you earlier: “I’ll never be able to get to sleep.” This is now proven wrong because you have managed to sleep. You’ve challenged the negative belief and won, because it’s no longer true!
This eventually helps to change your mindset, creating a positive association between bed and sleep, where going to bed is no longer associated with a battle to fall asleep.4
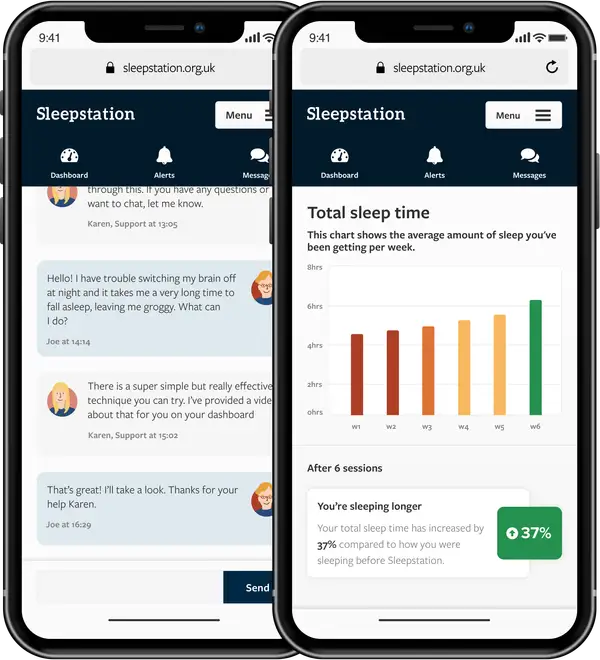
Sleep better with our support
Good support is key when you’re trying to fix your sleep especially if you’re using sleep restriction. At Sleepstation, our sleep coaches are on hand to support and guide you on your journey back to good sleep.
How sleep restriction therapy works in practice
Because sleep restriction therapy is administered differently depending on individual circumstance, exactly what treatment looks like will depends on a number of things, such as:
It’s important to work with a good sleep therapist either in person or over the internet, using a service like Sleepstation, so that you get the best outcome possible.6
Getting started with sleep restriction therapy usually follows these steps:
- You’ll have an appointment to see if sleep restriction therapy can help you.
- You’ll then be asked to complete a sleep diary across a few weeks that tracks:
- Based on this information, your therapist will set the total time permitted in bed. This is typically the average time you are actually asleep and no less than five hours per night to prevent excess fatigue.2
The times that are set for going to and getting out of bed depend on the type of insomnia that you have:
- if you have trouble falling asleep, a later bedtime is likely to be recommended
- if you can fall asleep easily but wake up too early, then bedtime is unaffected but an earlier time will be set to get out of bed.7
You then follow the schedule until you and your therapist agree there’s a consistent increase in the time spent asleep versus the total time you’ve spent in bed. At this point, more time in bed will be permitted.
Once out of your bed for the day, you shouldn’t lie down, nap or be in bed at all until the next scheduled bedtime.
Throughout the process, you’ll be regularly monitored, so that adjustments to the sleep schedule are easily made. Treatment is usually completed within a few months.
The long-lasting effects of sleep restriction therapy
Unlike a course of sleeping pills, sleep improvements from a course of sleep restriction therapy last for a number of months after treatment, with studies reporting consistent increases in the time in bed spent asleep and fewer awakenings while in bed.1389 10
Many people report that their attitudes towards sleep and going to bed have changed because of the long-lasting sleep improvements resulting from sleep restriction therapy.10
Perhaps unsurprisingly, brain scans of some people with insomnia who have undergone sleep restriction therapy show brain activity that is closer to that of good sleepers while in deep sleep. This suggests that the long-lasting improvement to your sleep may be down to some physical changes in your brain.11
Plus, people who’ve completed sleep restriction therapy report improved mood, reduced daytime fatigue, fewer sleep worries and napping tendencies compared to when they went untreated.12

Most importantly, sleep restriction therapy can be successfully used as part of a wider array of non-pharmacological treatments on a diverse range of people.
These include people who have lived with insomnia for several years, those with complex mental health issues, and the elderly.29 13
So, no matter how severe your insomnia is, or how long you’ve been experiencing a sleep problem, sleep restriction therapy as part of a course of CBTi is very likely to help you.
The first few weeks
It’s important to know what to expect when you begin your sleep restriction therapy. As your body adjusts to your new sleep schedule, you might experience daytime sleepiness, reduced alertness, mood disturbance and find working or socialising more difficult.14 Some of these effects could be down to your underlying insomnia, rather than the sleep restriction therapy, and these early effects should resolve as your sleep improves. 15
It’s during these early weeks that many people find it hard to succeed on their own. It’s so important to have the right support available, just when you need it. And that’s why at Sleepstation you have access to a team of sleep coaches and therapists every step of the way.
Your dedicated sleep team will regularly check-in with you and you can also message them at any time. And knowing that support is on hand can make a real difference when it comes to staying committed and achieving your goals.
Sleep restriction therapy tips
We want to arm you with all of the best tools and strategies to succeed. So, to help, we’ve pulled together some of our top tips to help you stay the course and get the very best results from your sleep restriction therapy.
- Acknowledge that willpower is key to this process. Getting into the right frame of mind from the start is going to improve your chances of success. Try and begin your therapy with the mindset that the effort you put in now will be worth the results you see in the end!
- Try to avoid napping. If you feel yourself nodding in the day, then get up and take a break from whatever you were doing. Even if it’s only to walk around the room to wake you back up, try removing yourself from the situation where napping is possible.
- Get exposure to sunlight. Natural light helps to set your body clock, so being outdoors in the daytime signals to your brain that this is the time to be awake and alert. If you take a walk outside every day, then the benefit is doubled as exercise is great for your health and wellbeing and may benefit your sleep too.
- Embrace routine. Sleep loves routine, so adopting a consistent wind-down routine can help to create associations in the brain that bedtime is coming and it’s time to get ready to sleep.
- Create a calm and cosy sleep environment. Your bedroom shouldn’t be a place for watching movies or catching up on your social media feeds. Your bedroom should be your sleep sanctuary, and we have lots of ideas to help you create the ideal bedroom setup.

These tips can make a big difference while you engage in your sleep restriction therapy but, as we said earlier, having real, human support will make you that much more likely to reach your goals.
And that’s where Sleepstation comes in.
Sleepstation can help you take back control of your sleep
At Sleepstation, we use a form of Cognitive Behavioural Therapy for insomnia (CBTi). Sleep restriction therapy makes up one of the core pillars of this therapy and, as we said earlier, we know that having good support throughout this process is absolutely key.
If you’re experiencing problems sleeping and would like to improve your sleep, we may be able to help. Sleepstation offers a highly effective solution to your sleep problem, tailored to you, the individual, with sustainable results. You can get started in just a few clicks, so why wait?

Summary
- Negative beliefs about sleep and being in bed are thought to make insomnia worse.
- Sleep restriction can help reset your brain’s focus away from being awake in bed to associating bed with sleep.
- This breaks the link between negative beliefs and poor sleep, helping you to sleep better.
- If you want to be supported through sleep restriction therapy and other key techniques of CBTi, Sleepstation can help.
References
- Falloon K, Elley CR, Fernando A 3rd, Lee AC, Arroll B. Simplified sleep restriction for insomnia in general practice: a randomised controlled trial. Br J Gen Pract 2015; 65: e508-15. ↩︎
- Morin CM, Hauri PJ, Espie CA, Spielman AJ, Buysse DJ, Bootzin RR. Nonpharmacologic treatment of chronic insomnia. Sleep 1999; 22: 1134–1156. ↩︎
- Friedman L, Benson K, Noda A, Zarcone V, Wicks DA, O’Connell K et al. An actigraphic comparison of sleep restriction and sleep hygiene treatments for insomnia in older adults. J Geriatr Psychiatry Neurol 2000; 13: 17–27. ↩︎
- Glovinsky PB, Spielman AJ. Sleep Restriction Therapy. In: Case Studies in Insomnia. Springer US: Boston, MA, 1991, pp 49–63. ↩︎
- Miller CB, Espie CA, Epstein DR, Friedman L, Morin CM, Pigeon WR et al. The evidence base of sleep restriction therapy for treating insomnia disorder. Sleep Med Rev 2014;18: 415–24. ↩︎
- Zachariae R, Lyby MS, Ritterband LM, O’Toole MS. Efficacy of internet-delivered cognitive-behavioral therapy for insomnia – A systematic review and meta-analysis of randomized controlled trials. Sleep Med Rev 2016; 30: 1–10. ↩︎
- Michael J, Sateia D. Insomnia: Diagnosis and treatment. 1st Edition. CRC Press: London, England, 2019. ↩︎
- Sivertsen B, Omvik S, Pallesen S, Bjorvatn B, Havik OE, Kvale G et al. Cognitive behavioral therapy vs zopiclone for treatment of chronic primary insomnia in older adults: a randomized controlled trial: A randomized controlled trial. JAMA 2006; 295: 2851–2858. ↩︎
- Breitstein J, Penix B, Roth BJ, Baxter T, Mysliwiec V. Intensive sleep deprivation and cognitive behavioral therapy for pharmacotherapy refractory insomnia in a hospitalized patient. J Clin Sleep Med 2014; 10: 689–690. ↩︎
- Kyle SD, Morgan K, Spiegelhalder K, Espie CA. No pain, no gain: an exploratory within-subjects mixed-methods evaluation of the patient experience of sleep restriction therapy (SRT) for insomnia. Sleep Med 2011; 12: 735–747. ↩︎
- Smith MT, Perlis ML, Chengazi VU, Soeffing J, McCann U. NREM sleep cerebral blood flow before and after behavior therapy for chronic primary insomnia: preliminary single photon emission computed tomography (SPECT) data. Sleep Med 2005; 6: 93–94. ↩︎
- Spielman AJ, Saskin P, Thorpy MJ. Treatment of chronic insomnia by restriction of time in bed. Sleep 1987; 10: 45–56. ↩︎
- Morin CM, Colecchi C, Stone J, Sood R, Brink D. Behavioral and pharmacological therapies for late-life insomnia: a randomized controlled trial. JAMA 1999; 281: 991–999. ↩︎
- Kyle SD, Miller CB, Rogers Z, Siriwardena AN, Macmahon KM, Espie CA. Sleep restriction therapy for insomnia is associated with reduced objective total sleep time, increased daytime somnolence, and objectively impaired vigilance: implications for the clinical management of insomnia disorder. Sleep 2014; 37: 229–237. ↩︎
- Whittall H, Pillion M, Gradisar M. Daytime sleepiness, driving performance, reaction time and inhibitory control during sleep restriction therapy for Chronic Insomnia Disorder. Sleep Med 2018; 45: 44–48. ↩︎