Key Points
Sexsomnia is recognised as a rare sleep disorder in which a person engages in sexual activity during their sleep. In general they’ll have no recollection of events during the act or when they wake up.
In this article, we’ve explored both the legal and medical sides of sexsomnia and we’ve covered the following areas:
- what is sexsomnia: we look at what sleep science can tell us about this rare disorder
- the causes of sexsomnia and how it can affect the individual and those around them
- how sexsomnia can be successfully treated by lifestyle changes and addressing underlying health conditions.
Introduction
Sexsomnia (often misspelled as ‘sexomnia’ and sometimes also known as ‘sleepsex’) is a rare sleep disorder which mostly affects men. It’s thought to account for around 7% of referrals to sleep disorders clinic, but the actual value is probably higher as some people may be embarrassed to seek help and others may not realise they have the problem.
Sexsomniacs engage in the following sexual activities while they’re asleep1:
- sexual vocalisations
- masturbation
- fondling
- intercourse/attempted intercourse.
Sexsomnia is considered a parasomnia, which means a sleep disorder related to abnormal movements.
There are many common parasomnias, and you’ve probably heard of ones such as sleepwalking, sleep paralysis and bedwetting (to name but a few).
Several parasomnias occur during our rapid eye movement (REM) sleep, a good example being sleep paralysis. REM sleep is generally considered to be when most of our dreams occur but sexsomnia occurs during non-REM sleep and isn’t related to dreaming.
As with other parasomnias, sexsomniacs do not remember the acts that they perform while they are asleep.
Although abnormal sexual behaviour during sleep was first described in 1989, the term ‘sexsomnia’ wasn’t coined until 2003 when 11 patients exhibiting sexual behaviours during sleep were described.2
Causes of sexsomnia
Sexsomnia can co-occur alongside other sleep disorders such as sleepwalking, sleep apnoea, night terrors and bedwetting. It may be triggered by:
- depression, stress and anxiety
- previous sleep deprivation
- poor sleep hygiene
- excessive consumption of alcohol or drugs
- use of sleeping tablets.
Treatments that improve the quality of sleep may help to reduce the incidence of events.
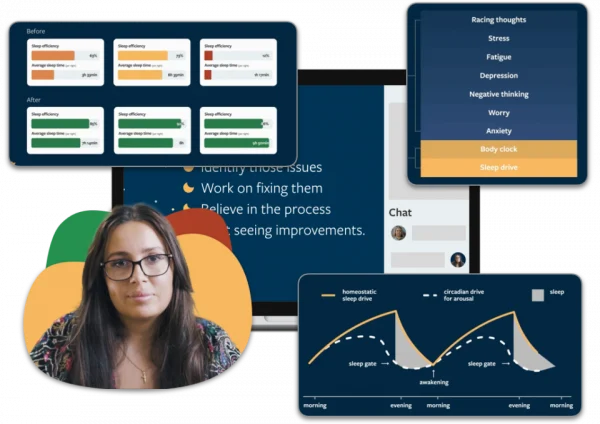
Cognitive Behavioural Therapy for insomnia (CBTi) can improve your sleep and mood.
When your sleep improves, it can also reduce levels of stress, anxiety and depression. If you’re having trouble sleeping and you feel like it’s having an effect on your mental and physical wellbeing, Sleepstation’s CBTi programme can help.
The implications of sleepsex
Sexsomnia, by its very nature, can have a profound impact on both the person with the condition and their partners. As people with sexsomnia tend to have no recollection of the events, it can be scary and confusing to learn that they have been carrying out behaviours outside of their conscious control.
For the bed partner, a range of feelings can be expected emcompassing everything from fear to enjoyment. In 2000, groundbreaking work was published recording stories and experiences of people who had experienced ‘sleepsex’.3
In a loving relationship, it may be understood as ‘just one of those things that happens’ as the account below suggests:
Sleepsex is great. My husband initiates it while we’re sleeping and then we wake up in the middle of making love. Often it’s better when he’s asleep because we’re completely relaxed and uninhibited.
However, given the nature of the behaviour, it may be hard for the bed partner to understand the fact that this behaviour is not deliberate:
During his sleepsex episodes, he becomes very aggressive and violent and then claims he does not remember anything… I had to call 911 last night because of a violent assault.
In extreme cases, sexsomnia has led to accusations of sexual assault — including rape — although the condition has been used successfully as a legal defence in some such cases.
A diagnosis of sexsomnia can often leave a person feeling shame, guilt or depression. For both the person experiencing sexsomnia and their partner, it’s crucial to speak to a sleep specialist and often consulting with a therapist may be recommended to help both parties with the diagnosis.
How is sexsomnia diagnosed?
Diagnosing sexsomnia usually relies on completing a sleep study, to try to capture the behaviour as it happens, or having accounts from a partner which, if detailed enough, can be sufficient for a doctor to determine if the behaviour is truly sleepsex.
When a sleep study is undertaken to diagnose sexsomnia, a person will usually spend several nights sleeping at a sleep clinic. During the sleep study, several measurements are taken while you sleep, including:
- brainwave activity
- heart rate and respiration rate
- leg and eye movements.
These can be used to identify or rule out other sleep disorders and ultimately accurately diagnose sexsomnia. If an episode of sexsomnia doesn’t occur during the sleep study then your doctor may recommend undertaking a second study.
Sexsomnia treatment approaches
Sexsomnia is treatable. As sexsomnia can be caused by other underlying sleep disorders, such as obstructive sleep apnoea, treating the primary cause should also help to resolve the sexsomnia.
Reducing intake of alcohol and addressing substance abuse in those with sexsomnia can be beneficial. Taking steps to reduce levels of stress, anxiety and depression can also have a positive effect on sexsomnia. Improving sleep hygiene can reduce symptoms.
Identifying measures to improve the overall sleep of someone with sexsomnia should help to reduce their sleep-sex symptoms.
As mentioned earlier, in some instances, talking therapies may be advised to help with processing any negative emotions that a person may be experiencing after receiving a diagnosis of sexsomnia.
If you think you may be experiencing sexsomnia, it’s important that you speak to your healthcare provider about it. Whether your worries are justified or not, leaving them unaddressed could interfere with your sleep and could lead to developing other sleep disorders, such as insomnia.
If you’re looking for sleep advice or want to learn more about how to sleep well, we have a wealth of information available in our articles section, ranging from sleep tips to the science behind everything sleep-related.
And if you’re worried about your sleep or a sleep problem then we can help. Sleepstation’s CBTi progamme is both clinically proven and highly effective, so if you want quality, long-lasting improvements to your sleep, based on decades of sound science, register for Sleepstation today.

Summary
- Sexsomnia is a relatively rare sleep disorder in which the person initiates sexual behaviour while asleep.
- Numerous causes and triggers of sexsomnia have been identified.
- Sexsomnia can be treated by addressing any underlying sleep problems and triggers.
References
- Andersen ML, Poyares D, Alves RS, Skomro R, Tufik S. Sexsomnia: abnormal sexual behaviour during sleep. Brain Research Reviews 2007;56:271–282 ↩︎
- Shapiro CM, Trajanovic NN, Fedoroff JP. Sexsomnia—a new parasomnia? The Canadian Journal of Psychiatry 2003;48:311–317. ↩︎
- Mangan M. Sleepsex: Uncovered. Xlibris Corporation; 2001. ↩︎