Key points
Zopiclone is a drug that’s often used for the short-term treatment of insomnia. In this article we look at what’s known about this sleep medicine and whether it is useful for people with insomnia. We’ll cover the following points:
- how zopiclone works
- can it help you sleep?
- withdrawal and addiction risks of zopiclone
- how to improve your sleep without medication.
Introduction
Zopiclone is one of the so-called “Z drugs”, along with zolpidem and zaleplon, and was introduced during the second half of the 1980s as a treatment for insomnia.
These drugs were developed as safer alternatives to benzodiazepines which can be highly addictive and whose use can lead to dependence.
Zopiclone was the first compound developed with a different chemical structure to the benzodiazepines but which binds to the same cell receptors as they do.1
It’s often called a short-acting hypnotic because of how quickly it’s eliminated from the body. It has a ‘half-life’ of about 5 hours (range of 3.5-6.5 hours), which refers to how long it takes for the concentration of the drug to be reduced by half in the body. In the elderly, the half-life is slightly longer, at around 7 hours.
Sleep better without zopiclone
People who have sleeping problems often turn to zopiclone , hoping for a quick fix. Most people don’t realise that there are more effective ways to treat your sleeping issues without side effects. With Sleepstation you can significantly improve your sleep without relying on medication. Sleepstation will help you:
- fall asleep quickly
- get all the sleep you need
- spend less time awake in bed
- wake feeling refreshed.
Sleep better without zopiclone
Get support from sleep experts, plus self-help tools.
Working with an expert who really grasps your situation is key to unlocking real sleep, effortless sleep. You deserve to sleep well and to work with people who have the right knowledge and expertise to help you get there.
Begin your journey to a lifetime of better sleep with:
- a full week of unlimited access to our highly-trained sleep coaches.
- direct contact and professional advice, with no waiting lists.
- expert insights to control and repair your sleep.
- lifetime access to an ever-growing library of sleep tools and resources.
What’s the recommended dose?
Zopiclone is licensed in the UK for adults with a bedtime dose of 7.5mg once daily for up to four weeks.
In the elderly, the initial dose is 3.75mg once daily, for up to four weeks. This can be increased, if necessary, to 7.5 mg daily.
These doses have been found to result in sedating and sleep-promoting effects similar to other benzodiazepine sleeping pills. You can find more information about Zopiclone from the NICE website.
It’s usually prescribed for short-term use (2-4 weeks) to limit the risk of your body becoming used to it and the drug losing its effectiveness.2 Short-term use is also advised to avoid you developing a dependence to it.
Zopiclone is available under the brand name Zimovane in the UK and Imovane or Rhovane in Canada. It’s not available for use in the United States although the related drug, eszopiclone, is on the US market.

How zopiclone affects sleep
Our sleep is made up of sleep cycles, which last for roughly 90 minutes and repeat several times throughout the night.
During each cycle, we pass through four different stages of sleep which are called N1, N2, N3 and rapid eye movement sleep (REM). When we fall asleep, we enter N1, then pass through N2 and N3 and finally into REM. The cycle then starts again at N1.
Zopiclone has been found to prolong stage N2 and N3 sleep with a proportional decrease in total REM sleep.3 Research also shows that it can reduce stage N1 sleep.4
However, many studies that have looked at sleeping brain activity in people who have taken zopiclone have shown results that are very variable, so all we can say with any certainty is that zopiclone can affect all stages of sleep.
The side effects of taking zopiclone
The most frequently reported side effect of zopiclone, reported in about 10% of people, is a bitter or metallic taste.5
Other frequently reported side effects of zopiclone include:
- nausea
- dizziness
- asthenia (abnormal physical weakness or lack of energy)
- increased sweating
- headaches
- sedation, somnolence and tiredness.
A study in healthy volunteers found no residual effects of the drug on psychomotor performance (i.e. activities such as throwing a ball, using a tool or driving a car) the day after a 7.5mg dose.3
However, there are other reports that do show impairment as a measure of coordination and performance of skilled tasks.

Hypnotics are often prescribed to the elderly. There is however a concern that they may impair both balance and memory functions.
More adverse effects on how the drugs such as zopiclone tend to have more adverse effects in older people. These include cognitive processes such as being able to concentrate or remember things. Increased daytime fatigue is also reported more frequently in older people being treated for insomnia.
These drugs also tend to affect psychomotor functions more in the elderly too. This refers to carrying out everyday tasks which involve coordinated movement, such as driving a car, playing an instrument, sewing or throwing a ball.
A study compared the effect of three hypnotics — including zopiclone 3.75mg and placebo — in 49 healthy volunteers aged 65 years and above.6 All active drugs were found to have a negative effect on balance and also reaction time on a test of memory.
The effects of zopiclone were found to persist for 8-9 hours, suggesting a possibility of a reduction in function after waking the morning after a night-time dose.
What are the withdrawal symptoms associated with zopiclone?
One of the concerns surrounding the use of sleeping pills is the incidence of withdrawal symptoms after stopping taking the drugs.
Research has shown that when zopiclone is used at the appropriate clinical doses then withdrawal effects are negligible or considerably lower than those associated with benzodiazepines.5 7 8 9
A review of studies investigating discontinuation of zopiclone found no significant rebound effect on sleep and few withdrawal effects such as anxiety and vertigo.10
Whereas another study found that withdrawal reactions like headache, anxiety, or agitation occurred in only 0.05% of the individuals studied.11
While withdrawal symptoms are not common, they can include:
- sleep problems
- anxiety and depression
- confusion and agitation
- muscle aches and pains.
To limit the risk of withdrawal symptoms, it’s sometimes recommended that you should slowly reduce the amount of zopiclone you are taking instead of abruptly stopping taking the drug, but this is something you should discuss with your healthcare provider.

Is zopiclone addictive?
If Zopiclone is taken regularly for an extended period of time, a person can build up a tolerance to it and would require higher doses to help them sleep. This is why the drug is generally recommended as only a short-term treatment option for insomnia.
Sleeping tablets are often associated with the risk of dependency or addiction, however, dependence on zopiclone is more often reported when the drug is taken at higher than prescribed doses and in people with a history of drug or alcohol abuse.
The presence of mental health problems, such as depression, has also been found to be a significant predictor when considering whether someone could become dependent.
So while the zopiclone does have the potential to lead to addiction, when it’s taken as a short-term treatment and at the recommended dose, it is considered quite safe.
Can zopiclone cause road accidents?
The effect of zopiclone on driving ability in the morning — following a night-time dose — has been investigated.
In a task simulating the anticipation of collision at an intersection, zopiclone (7.5mg) was found to have had no residual effect in 10 healthy and experienced drivers 10 hours after taking the drug.12
However, research has also shown that a single night-time dose of zopiclone (7.5mg) caused marked residual impairment in a highway driving test and on tests of attention and memory.13
These findings led the authors to conclude that patients should avoid driving the morning after taking zopiclone.
A further study by the same research group found that zopiclone impairs driving ability 10-11 hours after intake at a level that’s equivalent to the drink driving limits used in most European countries.14
While these studies were all conducted with healthy volunteers, research that examined the effect of single and repeated doses of zopiclone on driving performance in 23 insomnia patients found impaired performance 9-11 hours after taking the drug.15

In another study, the prescription records of more than 400,000 individuals were linked to police records of car crashes that involved almost 20,000 drivers.16
In this cohort, 14 cases were identified where zopiclone was associated with a road accident. However, this may be related to drug misuse.
A study in Norway showed that of the 101 drivers thought to be intoxicated and who had tested positive for zopiclone, 60 % of them had blood levels of zopiclone above those seen after taking the standard clinical dose.17
Eighty per cent were found to have higher than expected levels eight hours after intake of the drug.
It’s generally not recommended to drive within 12 hours of taking zopiclone. If the drug makes you feel dizzy or sleepy the following morning, or affects you in any other way that you think may impair your ability to drive, then you should not drive until you feel fit to do so.
Zopiclone, sleepwalking and other associated behaviours
Several reports have implicated zopiclone in causing sleepwalking and other atypical nocturnal behaviours including:
Patients experiencing these events have no memory of their actions but it’s debatable whether zopiclone is the sole cause.
It’s been reported that the use of alcohol and other CNS depressants, in conjunction with zopiclone, are associated with an increased risk of such behaviours.21
In some cases, zopiclone was used at levels exceeding the maximum recommended dose.
Caution concerning its possible hangover effects in the morning should be considered when deciding whether it’s the most appropriate drug for you and the lifestyle you lead.

Variations of zopiclone
Eszopiclone (Lunesta) is a variation of zopiclone approved in the United States in 2004. Although eszopiclone is supposed to have equivalent efficacy with zopiclone — and possibly an improved side effect profile — it’s not sold in the European Union or the UK.
A six-month study focused on the use of eszopiclone (3mg daily) in 593 patients aged 21-69 with primary insomnia.22
Results showed that eszopiclone significantly improved all self-reported sleep measures by:
- reducing how long it took to get to sleep
- increasing total sleep time
- reducing the number of awakenings
- improving sleep quality.
This study also found no evidence of tolerance to the effects of eszopiclone.
Patients’ rating of daytime alertness was better than with the placebo group and adverse event rates after discontinuation were not measurably different.
Should you take zopiclone to fix your sleep problems?
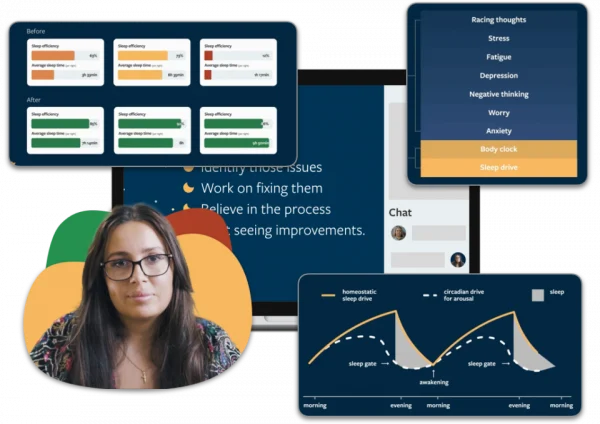
As a short-term treatment for insomnia, zopiclone does have some utility. It can help you to sleep, but it won’t get the root of why you were sleeping badly in the first case. The most effective way of treating insomnia long-term is cognitive behavioural therapy for insomnia (CBTi).
This is what we use in our online sleep clinic at Sleepstation. It’s a technique that helps you to identify and correct the behaviours and thought which lead to insomnia. What’s more, it’s highly effective and the effects last long after the programme is completed.
It’s not a short-term fix, like a sleeping tablet. It’s a programme that equips you with all the tools you need to take control of your sleep and tackle any further sleep problems should they arise.
So while sleeping tablets can be useful, they are not a solution to a sleep problem. Starting a programme with Sleepstation is quick and easy. Answer a couple of short questions and you can find out how Sleepstation can help you to overcome your sleep issues, drug-free, today.
Summary
- Zopiclone was created as a safer alternative to benzodiazepines.
- It’s used as a short-term treatment for insomnia and is usually prescribed for up to 4 weeks.
- Various hangover effects may occur with this drug, such as impairing your ability to drive the next day.
- It does not provide a long-term solution to insomnia, but may offer some relief of symptoms in the short-term.
- Sleepstation’s CBTi programme is drug-free and clinically-validated which has been proven to improve sleep, with sustainable results.
References
- Blanchard JC, Boireau A, Garret C, Julou L. In vitro and in vivo inhibition by zopiclone of benzodiazepine binding to rodent brain receptors. Life Sci 1979;24:2417–20. ↩︎
- Zopiclone: a sleeping pill used to treat bouts of insomnia [Internet]. nhs.uk. 2021 [cited 18 October 2021]. Available from: https://www.nhs.uk/medicines/zopiclone/ ↩︎
- Hemmeter U, Müller M, Bischof R, Annen B, Holsboer-Trachsler E. Effect of zopiclone and temazepam on sleep EEG parameters, psychomotor and memory functions in healthy elderly volunteers. Psychopharmacology (Berl) 2000;147:384–96. ↩︎
- Stone BM, Turner C, Mills SL, Paty I, Patat A, Darwish M, Danjou P (2002). Noise-induced sleep maintenance insomnia: hypnotic and residual effects of zaleplon. Br J Clin Pharmacol 53: 196-202. ↩︎
- Wadworth AN, McTavish D. Zopiclone: A review of its pharmacological properties and therapeutic efficacy as an hypnotic. Drugs Aging 1993;3:441–59. ↩︎
- Allain H, Bentué-Ferrer D, Tarral A, Gandon J-M. Effects on postural oscillation and memory functions of a single dose of zolpidem 5 mg, zopiclone 3.75 mg and lormetazepam 1 mg in elderly healthy subjects. A randomized, cross-over, double-blind study versus placebo. Eur J Clin Pharmacol 2003;59:179–88. ↩︎
- Wagner J, Wagner ML. Non-benzodiazepines for the treatment of insomnia. Sleep Med Rev 2000;4:551–81. ↩︎
- Lader M. The consequences of zopiclone use: rebound insomnia, development of tolerance, and abuse potential. Reviews in Contemporary Pharmacotherapy 1998;1;9(2):131-40. ↩︎
- Lader M. Withdrawal reactions after stopping hypnotics in patients with insomnia. CNS Drugs 1998;10:425–40. ↩︎
- Bianchi M, Musch B. Zopiclone discontinuation: review of 25 studies assessing withdrawal and rebound phenomena. Int Clin Psychopharmacol 1990;5 Suppl 2:139–45.
↩︎ - Inman W, Kubota K, Pearce G, Welton L. PEM report number 10. Zopiclone. Pharmacoepidemiol Drug Saf 1993;2:499–521. ↩︎
- Berthelon C, Bocca ML, Denise P, Pottier A. Do zopiclone, zolpidem and flunitrazepam have residual effects on simulated task of collision anticipation? J Psychopharmacol 2003;17:324–31. ↩︎
- Vermeeren A, Riedel WJ, van Boxtel MPJ, Darwish M, Paty I, Patat A. Differential residual effects of zaleplon and zopiclone on actual driving: a comparison with a low dose of alcohol. Sleep 2002;25:224–31. ↩︎
- Verster JC, Veldhuijzen DS, Volkerts ER. Residual effects of sleep medication on driving ability. Sleep Med Rev 2004;8:309–25. ↩︎
- Staner L, Ertlé S, Boeijinga P, Rinaudo G, Arnal MA, Muzet A, et al. Next-day residual effects of hypnotics in DSM-IV primary insomnia: a driving simulator study with simultaneous electroencephalogram monitoring. Psychopharmacology (Berl) 2005;181:790–8. ↩︎
- Barbone F, McMahon AD, Davey PG, Morris AD, Reid IC, McDevitt DG, et al. Association of road-traffic accidents with benzodiazepine use. Lancet 1998;352:1331–6. ↩︎
- Bramness JG, Skurtveit S, Mørland J. Zopiklonfunn hos mange bilførere-tegn på feilbruk og misbruk. Tidsskrift for Den Norske Legeforening 1999. ↩︎
- Ferentinos P, Paparrigopoulos T. Zopiclone and sleepwalking. Int J Neuropsychopharmacol 2009;12:141–2. ↩︎
- Dolder CR, Nelson MH. Hypnosedative-induced complex behaviours : incidence, mechanisms and management: Incidence, mechanisms and management. CNS Drugs 2008;22:1021–36. ↩︎
- Wilson J, Qazalbash A, Mistry D. Zopiclone and Complex Sleep-related Behaviours. UBC Medical Journal 2011;1;2(2). ↩︎
- Pressman MR. Sleep driving: sleepwalking variant or misuse of z-drugs? Sleep Med Rev 2011;15:285–92. ↩︎
- Krystal AD, Walsh JK, Laska E, Caron J, Amato DA, Wessel TC, et al. Sustained efficacy of eszopiclone over 6 months of nightly treatment: results of a randomized, double-blind, placebo-controlled study in adults with chronic insomnia. Sleep 2003;26:793–9. ↩︎