What is zolpidem, why’s it used and what’s the recommended dose?
Zolpidem is a sleeping pill that’s routinely prescribed for the short-term treatment of insomnia.
It’s one of the so-called Z drugs, alongside zopiclone and zaleplon, which were originally developed as safer alternatives to benzodiazepines. Zolpidem is a hypnotic agent, which means that it can induce sleep.
In America, it’s more commonly known by the brand name Ambien and in the UK it’s also called Stilnoct. It’s only available on prescription.
The standard adult dose is 10mg daily for up to four weeks, with the drug to be taken at bedtime. However, 5mg daily for up to four weeks is recommended for the elderly. The NICE website has information on Zolpidem which you can find here.

How zolpidem works and how it might affect you
Zolpidem is a fast-acting medication, which usually begins to make you feel sleepy within an hour of taking it.
It’s considered to be a short-acting hypnotic, which means that while it may help you fall asleep quicker, it may not necessarily help you to sleep longer as its effects wear off fairly quickly.
Zolpidem decreases how long it takes to fall asleep, improves sleep quality, increases stage N2 and N3 slow-wave sleep and reduces night‐time awakenings.1
In healthy adults, a study showed that a 10mg dose of zolpidem:
- reduced the number of awakenings and wake after sleep onset (WASO)
- improved sleep efficiency
- improved most subjective sleep measures relative to placebo.
Psychomotor performance and subjective assessment of morning sleepiness and morning concentration were not affected.
In this study, people taking zolpidem did not become tolerant to the drug or experience a rebound effect (i.e. a recurrence of sleep problems with worse symptoms) after using the recommended dosage for five weeks.2
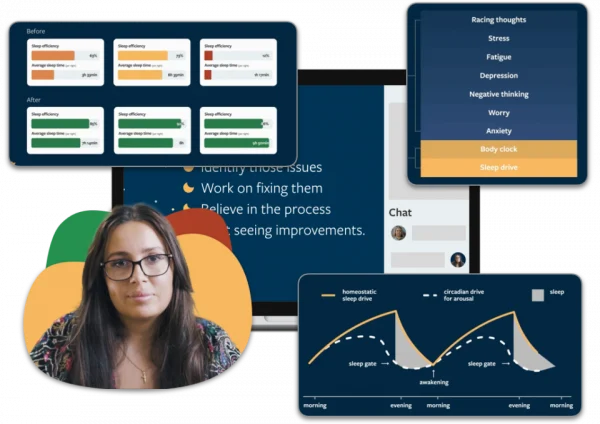
Sleep better without zolpidem
People who have sleeping problems often turn to zolpidem, hoping for a quick fix. Most people don’t realise that there are more effective ways to treat your sleeping issues without side effects. With Sleepstation you can significantly improve your sleep without relying on medication. Sleepstation will help you:
- fall asleep quickly
- get all the sleep you need
- spend less time awake in bed
- wake feeling refreshed.
Sleep better without zolpidem
Get support from sleep experts, plus self-help tools.
Working with an expert who really grasps your situation is key to unlocking real sleep, effortless sleep. You deserve to sleep well and to work with people who have the right knowledge and expertise to help you get there.
Begin your journey to a lifetime of better sleep with:
- a full week of unlimited access to our highly-trained sleep coaches.
- direct contact and professional advice, with no waiting lists.
- expert insights to control and repair your sleep.
- lifetime access to an ever-growing library of sleep tools and resources.
Zolpidem can be taken in several different ways
Zolpidem can be prescribed as a pill, in a form that dissolves under the tongue or as a mouth spray.
It’s also available in a modified formulation that leads to an extended release of the drug during the night. We’ll have a look at the different formulations and why they were developed.
Modified‐release (MR) formulation of zolpidem
Because of its short duration of action and inconsistent effects on sleep maintenance, a modified-release version of zolpidem has been developed that releases the drug throughout the night.
Zolpidem‐MR has been marketed in the United States since 2005 — somewhat confusingly under the name Ambien CR.
Zolpidem-MR is a two-layered tablet. It has one layer that’s released immediately after taking it, which leads to a zolpidem concentration in the body similar to the original formulation.
This is followed by the second layer, which provides an extended release of zolpidem to maintain levels of the drug through the middle of the night.
The dosage is also slightly different to that of the standard formulation, with the starting dose of Zolpidem-MR being 12.5mg for adults and 6.25mg for the elderly.3
This formulation is intended to help people who wake in the night, as it provides a longer release of zolpidem.
A study found that Zolpidem-MR at 12.5mg provided sustained and significant improvements in sleep onset and maintenance and improved next‐day concentration and morning sleepiness for up to six months.4
Zolpidem-MR has a safety profile comparable to the original, immediate-release formulation. and has not been shown to significantly affect psychomotor and cognitive performance eight hours post-dose.5 6

Zolpidem as a sublingual tablet
Zolpidem is also available as a sublingual tablet that is placed under the tongue and allowed to dissolve completely before swallowing.
Common brand names of this form include Edluar and Intermezzo. Zolpidem for sublingual use is not to be swallowed whole and shouldn’t be taken with or immediately after a meal.
This mode of drug delivery allows zolpidem to be used to treat middle-of-the-night insomnia when an awakening is followed by difficulty returning to sleep.
However, it shouldn’t be taken if you have less than four hours of sleep time remaining, as it could interfere with your daily functioning if taken too close to when you wake up.
Zolpidem as an oral mist
Zolpidem oral mist (brand name ZolpiMist) is also available. This formulation is sprayed into your mouth and over your tongue, usually once a night, and provides an alternative way of taking the drug.7
It should be taken just before you get into bed. Unlike the sublingual tablets, this product is not for use in the middle of the night and should only be used if you have time for a whole night’s sleep of at least 7-8 hours.
The recommended dose is no higher than 10mg a day — the same as the standard zolpidem tablets.

Is zolpidem a safe way to treat sleep problems?
Numerous studies have demonstrated a good safety profile for zolpidem compared to benzodiazepine-class drugs. It’s a safe and effective drug when taken at the recommended dosage.
Zolpidem is however known to interact with drugs that primarily have sedative properties. Current NHS guidelines state that you should check with your healthcare provider or pharmacist if you are already taking:
- drowsy antihistamines such as chlorphenamine or promethazine
- medicines to treat schizophrenia and bipolar disorder
- medicines to treat depression
- medicines for epilepsy
- medicines to calm or reduce anxiety
- medicines for sleep problems
- medicines used to treat fungal infections (such as ketoconazole and itraconazole)
- ritonavir (a medicine used to treat HIV infections)
- strong painkillers (such as codeine, methadone, morphine, oxycodone, pethidine or tramadol).8
Due to concerns over tolerance, dependence and withdrawal effects, the current NICE guidelines do not recommend the use of any hypnotic drugs, including zolpidem, for periods of more than four weeks.
Longer term use of zolpidem
While it’s advised only to be used in the short term, several studies suggest that zolpidem in the dose range of 5 -10mg is safe even for extended treatment periods.9
One study looked at the effects of taking zolpidem nightly for eight months as a treatment for primary insomnia. The results showed that the drug stayed effective at improving the sleep of participants during this period, without tolerance to the drug becoming an issue.9 10
Further research on the extended use of zolpidem has shown no clinically significant withdrawal symptoms after 12 months of nightly use.10
In this work, the authors concluded that chronic nightly use of zolpidem, at therapeutic doses by people with primary insomnia, does not lead to rebound insomnia or withdrawal symptoms after treatment was over.
One of the issues with many sleeping tablets is the potential for tolerance to the effects of the drug, which leads to people needing to take higher and higher doses of the medication to get the same effect.
However, a study has shown that chronic use of zolpidem by primary insomniacs did not lead to dose escalation during 12 months of nightly use,10 suggesting a low potential for tolerance in this time frame.
The side effects of zolpidem
There are numerous side effects associated with taking this drug. Common or very common side effects of zolpidem include:
- abdominal pain
- anterograde amnesia
- anxiety
- back pain
- diarrhoea
- dizziness
- fatigue
- hallucination
- headache
- increased risk of infection
- nausea
- sleep disorders
- vomiting.11
Less common side effects include poor motor coordination, difficulty maintaining balance, increased appetite, increased libido, impaired judgment and reasoning.12 13

Zolpidem and older people
A limited amount of data indicates that the use of zolpidem by older people is associated with an increased risk of falls and resultant hip fractures.14
However, the evidence generally suggests that this risk is less when compared with those older people using benzodiazepine-class medications.
The relationship between hypnotic drug use and falls is complicated because untreated sleep problems among older adults are also associated with an increased risk of falls, meaning it’s hard to assign why these falls are happening.
However we do know that drug metabolism can often be slower as we age, hence why this drug is given at a lower dose in the older age group.
The hypnotic effect of zolpidem
Reports of bizarre sleep‐related behaviours have been linked to the use of zolpidem. These include:
- sleepwalking
- phone conversations
- hallucinations
- preparing and eating food
- house cleaning
- driving while asleep.
People exhibiting these sleep‐related behaviours report no memory of the event. In most cases, such behaviours resolved when zolpidem treatment was stopped.
Such side-effects are usually associated with taking more than the recommended dose of the drug, or taking it in combination with the use of alcohol or other CNS depressants.15 16

Zolpidem has also been shown to exert a hypnotic effect without disturbing psychomotor and physical performance the following day, when given to healthy adults.
Psychotic reactions with visual hallucinations following the ingestion of zolpidem have also been reported in the literature.17 18
Seizure is a rare and severe withdrawal symptom of zolpidem: it seems to occur in people who have taken higher than recommended doses for a long time and then abruptly stop taking the drug.19
Zolpidem has also been shown to exert a hypnotic effect without disturbing psychomotor and physical performance the following day, when given to healthy adults.
Zolpidem misuse
While zolpidem was developed as a safer alternative to benzodiazepines, and does retain this title, its use is not without its drawbacks.
Zolpidem was originally thought to have a very low potential for abuse and wasn’t considered to lead to dependence.
However, prescription and illegal use of the drug has increased dramatically over the years and it is often abused.20
More than 30 years after the drug became available, there’s now mounting evidence that addiction and dependence can arise from use of zolpidem.
In 2001, the USA’s food and drinks agency (FDA) recategorised the drug as a Schedule IV drug (one that causes dependence).
In light of accumulating evidence for dependence and misuse, France too re-evaluated their classification of the drug, bringing in greater controls over the prescribing of zolpidem.
America’s FDA has recently updated the information on this drug to give a stronger warning about complex sleep behaviours after taking zolpidem.
Its use is cautioned for people with a history of drug or alcohol problems and it should not be used at higher than the recommended dosage.
Zolpidem and CBTi
The use of zolpidem is only advised after non-pharmacological measures have been tried first. These measures can include improving sleep hygiene and completing a course of cognitive behaviour for insomnia (CBTi).
CBTi involves using a combination of behavioural and cognitive techniques to improve sleep habits and reduce sleep-disruptive behaviours and ideas.
It’s a drug-free method and is recommended as the first line approach to treating insomnia and sleep disorders.
The effectiveness of CBTi has been compared with the use of various sleeping tablets, and it’s been shown to be superior to medication for both improving sleep and maintenance of sleep improvement after treatment is completed.
Studies have directly compared the use of zolpidem with CBT approaches, including CBTi 21, with these non-drug treatment options being found to provide greater benefit than the drug.21 22 23
At Sleepstation, we use a form of CBTi that’s both clinically validated and backed by years of scientific research. We’ve successfully helped thousands of people to sleep better, without the need for drugs.
So if you’re looking to improve your sleep, without the use of medication, our digital sleep clinic has a range of services to help, based on how severe your sleep problem is and how much support you need. Read the evidence and find out how we can help you here.
Summary
- Zolpidem is one of the so-called Z drugs.
- It’s used to treat sleep problems in the short term.
- Zolpidem is fast-acting and has minimal residual and rebound effects when used as directed.
- Its safety record has been called into question due to evidence of dependency and abuse of the drug.
- Zolpidem can induce a hypnotic effect in healthy people as well as those living with insomnia.
- It’s still an effective alternative to benzodiazepines.
- CBTi should be considered as the first-line treatment before use of zoplidem.
References
- Monti JM. Effect of zolpidem on sleep in insomniac patients. Eur J Clin Pharmacol. 1989;36(5):461–6. ↩︎
- Walsh JK, Vogel GW, Scharf M, Erman M, William Erwin C, Schweitzer PK, et al. A five week, polysomnographic assessment of zaleplon 10 mg for the treatment of primary insomnia. Sleep Med. 2000;1(1):41–9. ↩︎
- Krystal AD, Erman M, Zammit GK, Soubrane C, Roth T, Group ZOLONGS. Long-term efficacy and safety of zolpidem extended-release 12. 5 mg, administered 3 to 7 nights per week for 24 weeks, in patients with chronic primary insomnia: a 6-month, randomized, double-blind, placebo-controlled, parallel-group, multicenter study. Sleep. 2008;31(1):79–90. ↩︎
- Hindmarch I, Legangneux E, Stanley N, Emegbo S, Dawson J. A double-blind, placebo-controlled investigation of the residual psychomotor and cognitive effects of zolpidem-MR in healthy elderly volunteers. Br J Clin Pharmacol. 2006;62(5):538–45. ↩︎
- Blin O, Micallef J, Audebert C, Legangneux E. A double-blind, placebo-and flurazepam-controlled investigation of the residual psychomotor and cognitive effects of modified release zolpidem in young healthy volunteers. Journal of clinical psychopharmacology. 2006;1;26(3):284-9. ↩︎
- Greenblatt DJ, Harmatz JS, Roth T, Singh NN, Moline ML, Harris SC, et al. Comparison of pharmacokinetic profiles of zolpidem buffered sublingual tablet and zolpidem oral immediate-release tablet: results from a single-center, single-dose, randomized, open-label crossover study in healthy adults. Clin Ther. 2013;35(5):604–11. ↩︎
- Neubauer DN. ZolpiMistTM: a new formulation of zolpidem tartrate for the short-term treatment of insomnia in the US. Nat Sci Sleep. 2010;2:79–84. ↩︎
- nhs.uk. 2021. Zolpidem: a sleeping pill used to treat insomnia. [online] Available at: https://www.nhs.uk/medicines/zolpidem/ [Accessed 20 September 2021]. ↩︎
- Randall S, Roehrs TA, Roth T. Efficacy of eight months of nightly zolpidem: a prospective placebo-controlled study. Sleep. 2012;35(11):1551–7. ↩︎
- Roehrs TA, Randall S, Harris E, Maan R, Roth T. Twelve months of nightly zolpidem does not lead to rebound insomnia or withdrawal symptoms: a prospective placebo-controlled study. J Psychopharmacol. 2012;26(8):1088–95. ↩︎
- NICE-The National Institute for Health, Excellence C. BNF: British national formulary – NICE. [cited 2021 Sep 20]; Available from: https://bnf.nice.org.uk/drug/zolpidem-tartrate.html ↩︎
- Dang A, Garg A, Rataboli PV. Role of zolpidem in the management of insomnia: Role of zolpidem. CNS Neurosci Ther. 2011;17(5):387–97. ↩︎
- Toner LC, Tsambiras BM, Catalano G, Catalano MC, Cooper DS. Central nervous system side effects associated with zolpidem treatment. Clin Neuropharmacol. 2000;23(1):54–8. ↩︎
- Wang PS, Bohn RL, Glynn RJ, Mogun H, Avorn J. Zolpidem use and hip fractures in older people. J Am Geriatr Soc. 2001;49(12):1685–90. ↩︎
- Inagaki T, Miyaoka T, Tsuji S, Inami Y, Nishida A, Horiguchi J. Adverse reactions to zolpidem: case reports and a review of the literature. Prim Care Companion J Clin Psychiatry [Internet]. 2010;12(6). ↩︎
- Daley C, McNiel DE, Binder RL. I did what?” Zolpidem and the courts. Journal of the American Academy of Psychiatry and the Law Online. 2011;1;39(4):535-42. ↩︎
- Ansseau M, Pitchot W, Hansenne M, Moreno A. Psychotic reactions to zolpidem. Lancet. 1992;339(8796):809. ↩︎
- Huang C-L, Chang C-J, Hung C-F, Lin H-Y. Zolpidem-induced distortion in visual perception. Ann Pharmacother. 2003;37(5):683–6. ↩︎
- Cubała WJ, Landowski J. Seizure following sudden zolpidem withdrawal. Progress in Neuro-Psychopharmacology and Biological Psychiatry. 2007;31(2):539–40. ↩︎
- Orsolini L, Chiappini S, Grandinetti P, Bruschi A, Testa R, Provenzano A, et al. ‘Z-trip’? A comprehensive overview and a case-series of zolpidem misuse. Clin Psychopharmacol Neurosci. 2021;19(2):367–87. ↩︎
- Mitchell MD, Gehrman P, Perlis M, Umscheid CA. Comparative effectiveness of cognitive behavioral therapy for insomnia: a systematic review. BMC Fam Pract. 2012;13(1):40. ↩︎
- Jacobs GD, Pace-Schott EF, Stickgold R, Otto MW. Cognitive behavior therapy and pharmacotherapy for insomnia: a randomized controlled trial and direct comparison:. Arch Intern Med. 2004;164(17):1888–96. ↩︎
- Wu R, Bao J, Zhang C, Deng J, Long C. Comparison of sleep condition and sleep-related psychological activity after cognitive-behavior and pharmacological therapy for chronic insomnia. Psychother Psychosom. 2006;75(4):220–8. ↩︎